Why The Body Attacks Itself After COVID-19 Vaccination?
Why the body attacks itself after covid 19 vaccination – Why The Body Attacks Itself After COVID-19 Vaccination? It’s a question that has sparked much discussion and concern, especially as more people receive the vaccine. While vaccines are designed to protect us from diseases, in rare cases, they can trigger an immune response that mistakenly targets the body’s own tissues.
This phenomenon, known as an autoimmune reaction, can manifest in various ways, from mild discomfort to more serious complications.
Understanding the intricacies of the immune system, the potential mechanisms behind these reactions, and the available evidence are crucial for addressing this concern. This article delves into the science behind autoimmune reactions following COVID-19 vaccination, exploring the potential risk factors, the available treatment options, and the importance of ongoing research in this field.
Understanding the Immune Response to COVID-19 Vaccination
Vaccines are a cornerstone of modern medicine, safeguarding us from a multitude of infectious diseases. The success of vaccines lies in their ability to prime our immune system to recognize and combat specific pathogens, ultimately preventing illness. COVID-19 vaccines, in particular, have proven to be highly effective in mitigating the severity of the disease and reducing the risk of hospitalization and death.
Understanding how these vaccines work, specifically how they trigger the immune response, is crucial for appreciating their efficacy and for addressing concerns about potential side effects.
The Normal Immune Response to Vaccines
Vaccines work by introducing a weakened or inactive version of a pathogen, or specific components of the pathogen, into the body. This “mock” infection triggers a robust immune response without causing the disease itself. The immune system, a complex network of cells and organs, is designed to protect us from foreign invaders.
When a vaccine is introduced, the immune system recognizes it as a threat and mounts a defense. This defense involves two key players: antibodies and T cells.
- Antibodies:These are proteins produced by specialized immune cells called B cells. Antibodies bind to specific targets on the pathogen, effectively neutralizing them and marking them for destruction by other immune cells.
- T cells:These are another type of immune cell that directly attack and destroy infected cells or cells that have become cancerous. T cells also play a role in regulating the immune response, ensuring that it is appropriately targeted and controlled.
Immune Responses Triggered by COVID-19 Vaccines, Why the body attacks itself after covid 19 vaccination
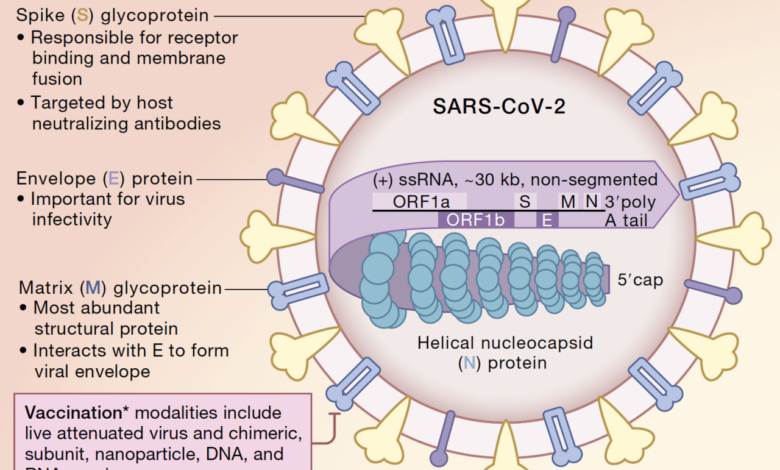
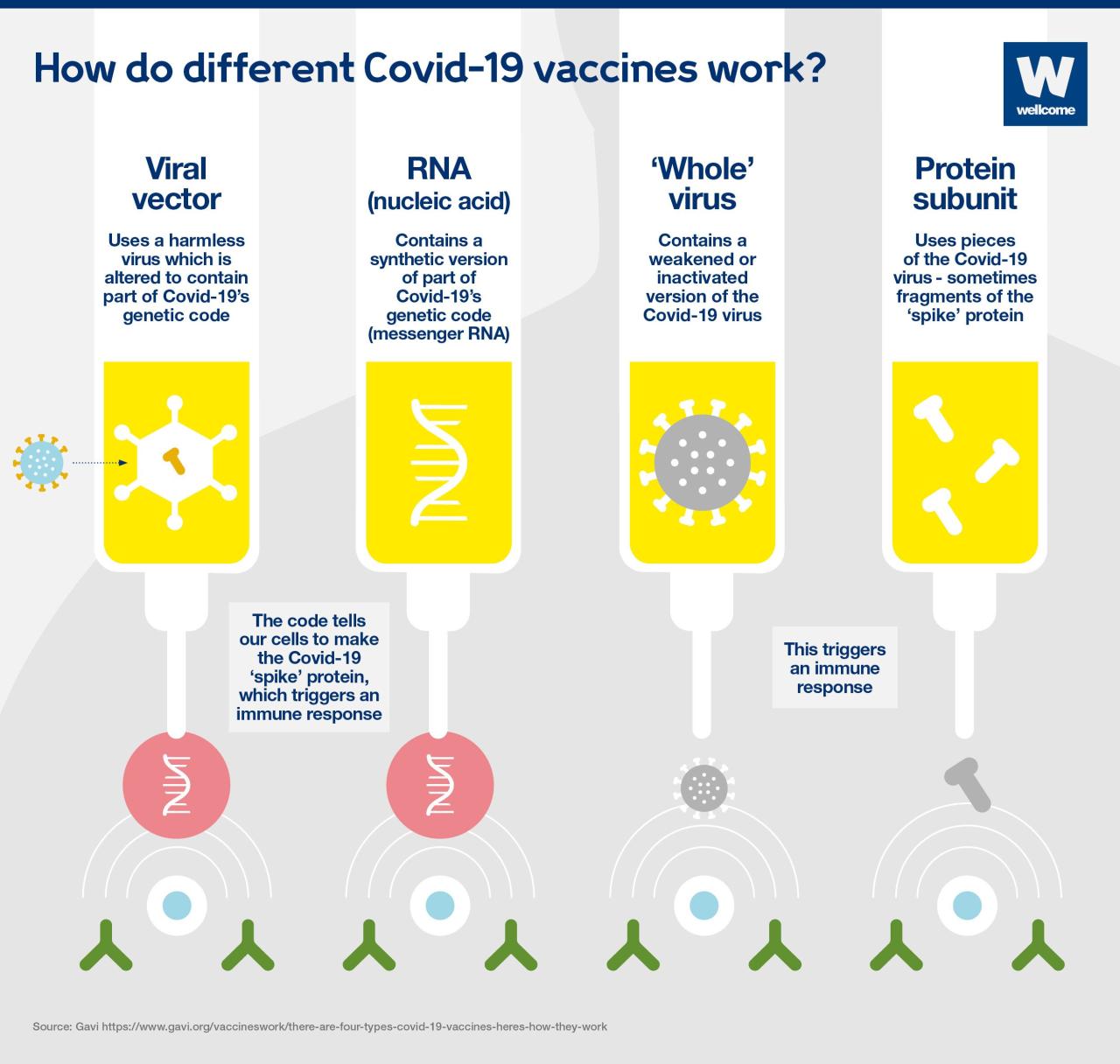
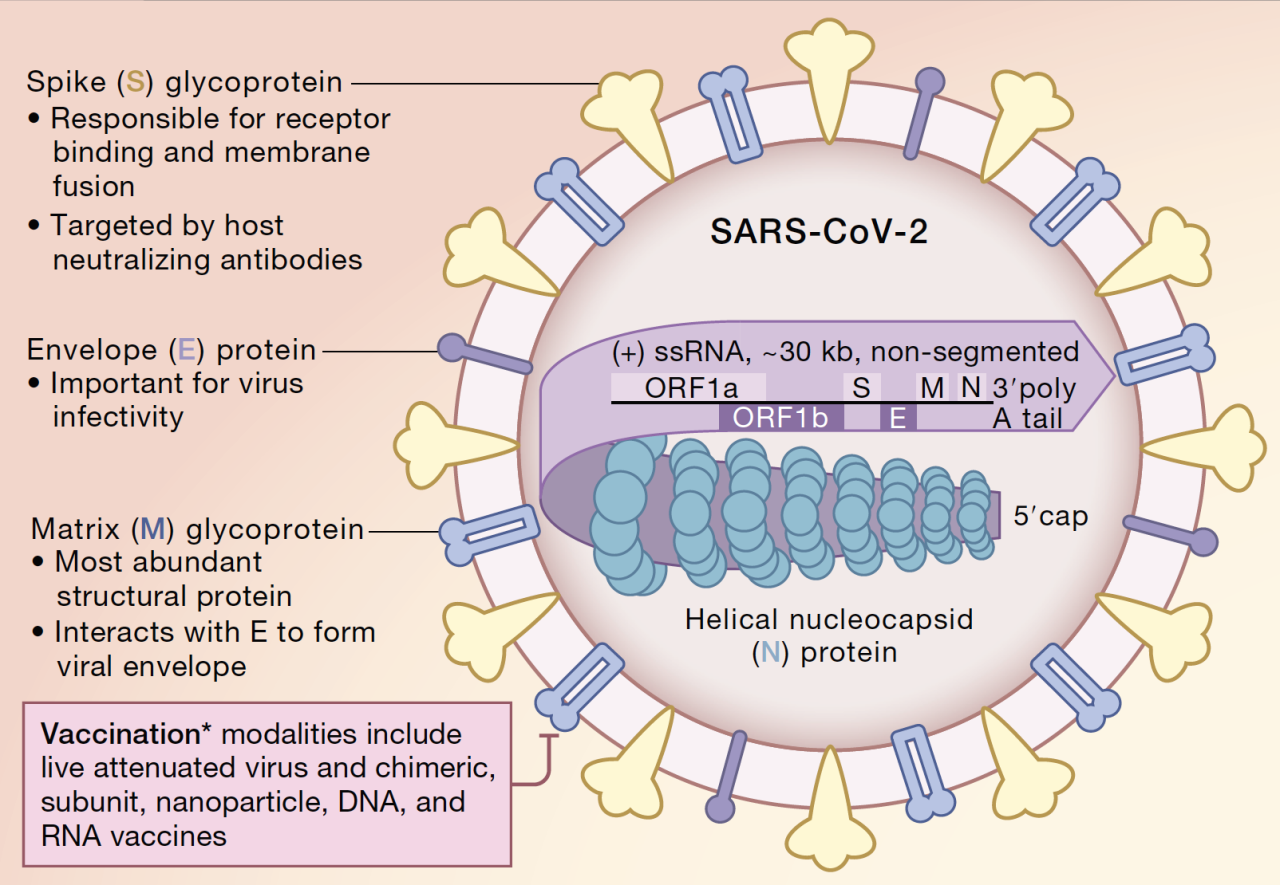
COVID-19 vaccines, like other vaccines, work by triggering the production of antibodies and T cells that specifically target the SARS-CoV-2 virus. The specific immune responses triggered by these vaccines vary depending on the vaccine type.
Comparing Immune Responses to Different COVID-19 Vaccines
COVID-19 vaccines fall into several categories, each utilizing different technologies to induce an immune response:
- mRNA Vaccines (Pfizer-BioNTech and Moderna):These vaccines deliver genetic instructions, in the form of mRNA, that teach cells how to produce a harmless piece of the spike protein found on the surface of the SARS-CoV-2 virus. This protein fragment is then displayed on the surface of cells, triggering the immune system to recognize and mount a defense against the virus.
- Viral Vector Vaccines (Johnson & Johnson and AstraZeneca):These vaccines use a modified, harmless virus (the vector) to deliver genetic instructions for the spike protein into cells. The vector itself cannot cause illness, but it carries the instructions for the spike protein, enabling the body to produce it and trigger an immune response.
- Protein-Based Vaccines (Novavax):These vaccines contain a purified, inactive version of the spike protein. This protein is recognized by the immune system, leading to the production of antibodies and T cells that can target the real virus.
| Vaccine Type | Mechanism of Action | Immune Response |
|---|---|---|
| mRNA Vaccines | Delivers mRNA encoding spike protein | Induces antibody and T cell responses against the spike protein |
| Viral Vector Vaccines | Uses a modified virus to deliver spike protein instructions | Induces antibody and T cell responses against the spike protein |
| Protein-Based Vaccines | Contains purified spike protein | Induces antibody and T cell responses against the spike protein |
Autoimmune Reactions and COVID-19 Vaccination
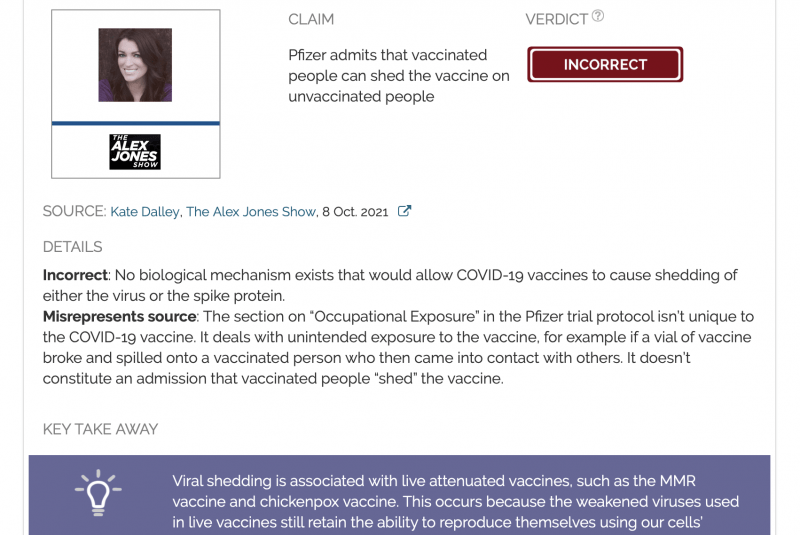
The vast majority of people who receive COVID-19 vaccines experience mild side effects, such as pain at the injection site, fatigue, or headache. However, there have been rare reports of autoimmune reactions following vaccination. This raises concerns about the potential for COVID-19 vaccines to trigger or exacerbate autoimmune disorders.
Autoimmune reactions occur when the immune system mistakenly attacks the body’s own tissues. This can lead to a range of symptoms, depending on the specific tissues involved.
It’s fascinating how the body can sometimes react to vaccines, like the COVID-19 shot, by mounting an immune response that seems to target itself. While this might sound scary, it’s often a temporary and manageable side effect. Speaking of regulations, the USDA is proposing a new rule for “Product of USA” food labels , which could impact how we understand the origins of our food.
Understanding these complex immune reactions, like those after vaccination, is crucial, and hopefully, the USDA’s new rule will bring more clarity to food labeling.
Potential Mechanisms of Autoimmune Reactions Following COVID-19 Vaccination
Several potential mechanisms could explain how COVID-19 vaccination might trigger autoimmune reactions.
- Molecular Mimicry:The spike protein of the SARS-CoV-2 virus, which is targeted by COVID-19 vaccines, shares some similarities with certain proteins found in the human body. This molecular mimicry could lead the immune system to mistakenly attack both the viral spike protein and the similar human proteins, triggering an autoimmune response.
- Bystander Activation:The immune response to vaccination can sometimes activate immune cells in a non-specific way. This bystander activation could potentially lead to the activation of autoreactive T cells, which are immune cells that target the body’s own tissues.
- Altered Immune Tolerance:Vaccines, like any foreign substance introduced into the body, can sometimes disrupt the delicate balance of immune tolerance, leading to an increased risk of autoimmune reactions.
Examples of Autoimmune Disorders Triggered by Vaccines
While rare, there are documented cases of autoimmune disorders being triggered by vaccines in general. Here are a few examples:
- Guillain-Barré Syndrome (GBS):This rare neurological disorder can be triggered by certain vaccines, including the influenza vaccine. GBS is characterized by muscle weakness and paralysis.
- Myocarditis:Inflammation of the heart muscle, has been linked to some vaccines, including the mRNA COVID-19 vaccines. However, it is important to note that myocarditis is also a known side effect of COVID-19 infection itself.
- Thrombocytopenia:A condition characterized by low platelet count, has been associated with the adenovirus-based COVID-19 vaccine (e.g., the Johnson & Johnson vaccine).
Evidence for Autoimmune Reactions Following COVID-19 Vaccination
The safety and efficacy of COVID-19 vaccines have been extensively studied, and they are generally considered safe and effective. However, like any medical intervention, there is a possibility of adverse effects, including autoimmune reactions. While these reactions are rare, understanding their potential occurrence is crucial for informed decision-making.This section explores the current scientific evidence regarding autoimmune reactions following COVID-19 vaccination.
We will examine studies that have investigated the link between COVID-19 vaccination and autoimmune disorders and discuss the limitations of current research and the need for further investigation.
Studies Investigating the Link Between COVID-19 Vaccination and Autoimmune Disorders
Several studies have investigated the potential link between COVID-19 vaccination and autoimmune disorders. These studies have employed various methodologies, including observational studies, case reports, and post-marketing surveillance data.
It’s fascinating how our immune system sometimes goes haywire after a COVID-19 vaccination, attacking our own cells. This might sound scary, but it’s actually a sign of a robust immune response. It’s similar to how some people react to a Nobel Peace Prize nomination – a bit of a shock, but ultimately a positive sign.
Trump reacted to his nomination with enthusiasm , calling it a great thing for the country. The body’s immune system, like a well-meaning but slightly overzealous friend, might be a little over the top in its response, but it’s all in the name of protecting us from future threats.
- Observational Studies:These studies have analyzed large datasets to assess the risk of developing autoimmune disorders after COVID-19 vaccination. For example, a study published in the journal -JAMA Network Open* analyzed data from over 12 million individuals in the US and found no increased risk of developing autoimmune disorders after receiving a COVID-19 vaccine.
However, it’s important to note that observational studies can only establish associations, not cause-and-effect relationships.
- Case Reports:Case reports document individual cases of autoimmune reactions following COVID-19 vaccination. While these reports provide valuable insights into potential adverse events, they are limited by their small sample size and the possibility of confounding factors. For instance, a case report published in the -Journal of Clinical Immunology* described a patient who developed Guillain-Barré syndrome after receiving a COVID-19 vaccine.
It’s a bit of a mind-boggler, isn’t it? Why would our own immune system turn against us after a COVID-19 vaccination? It’s like our body is confused, mistaking the vaccine for a real threat. It’s a complex process, but the main idea is that the immune system gets a bit overzealous and attacks healthy cells.
It’s even more frustrating when you consider that the Republicans in Congress, as highlighted in this article mccarthy dems would rather watch america suffer covid relief blocked , seem to be more interested in playing politics than in helping Americans recover from the pandemic.
It’s a shame that we can’t rely on our leaders to work together to address these complex issues, like the potential side effects of vaccines, and instead, we’re left to grapple with them on our own.
However, it’s important to emphasize that this does not necessarily imply a causal link.
- Post-Marketing Surveillance Data:Post-marketing surveillance systems collect data on adverse events reported after the authorization of a vaccine. The Vaccine Adverse Event Reporting System (VAERS) in the US is an example of such a system. While VAERS data can provide valuable information about potential safety concerns, it’s important to note that reports to VAERS are not necessarily evidence of a causal relationship between vaccination and an adverse event.
Limitations of Current Research
Despite the growing body of research, it’s important to acknowledge the limitations of current studies.
- Limited Sample Sizes:Many studies investigating the link between COVID-19 vaccination and autoimmune disorders have relatively small sample sizes, which can limit the generalizability of their findings.
- Confounding Factors:It can be challenging to isolate the effect of vaccination from other potential confounding factors, such as pre-existing health conditions or exposure to other viruses.
- Lack of Long-Term Data:The long-term effects of COVID-19 vaccination on autoimmune disorders are still being investigated. More time is needed to assess the potential for delayed or long-term reactions.
Need for Further Investigation
The potential for autoimmune reactions following COVID-19 vaccination warrants further investigation. Future research should focus on:
- Larger and More Robust Studies:Conducting larger and more robust studies with well-defined cohorts can provide stronger evidence on the link between COVID-19 vaccination and autoimmune disorders.
- Longitudinal Studies:Longitudinal studies that follow individuals over time can help assess the long-term effects of COVID-19 vaccination on autoimmune disorders.
- Mechanistic Studies:Mechanistic studies can investigate the biological mechanisms by which COVID-19 vaccination might trigger autoimmune reactions.
Risk Factors for Autoimmune Reactions After Vaccination
While COVID-19 vaccines are generally safe and effective, a small number of individuals may experience autoimmune reactions after vaccination. Understanding the risk factors associated with these reactions can help identify individuals who might be more susceptible and require closer monitoring.
Genetics
Genetics plays a significant role in the development of autoimmune diseases. Certain genes can increase an individual’s susceptibility to autoimmune reactions. For instance, the presence of specific human leukocyte antigen (HLA) genes has been linked to an increased risk of autoimmune disorders.
These genes influence the immune system’s ability to distinguish between self and non-self antigens, potentially leading to an autoimmune response.
Pre-existing Autoimmune Conditions
Individuals with pre-existing autoimmune conditions are at a higher risk of experiencing autoimmune reactions after COVID-19 vaccination. This is because their immune system is already primed to attack its own tissues, and vaccination may trigger a flare-up or exacerbate existing symptoms.
For example, individuals with rheumatoid arthritis, lupus, or inflammatory bowel disease might be more likely to develop autoimmune complications after vaccination.
Other Factors
Other factors can also contribute to the risk of autoimmune reactions after vaccination. These include:
- Age:Older adults may have a weakened immune system, making them more susceptible to autoimmune reactions.
- Sex:Women are generally more prone to autoimmune diseases than men.
- Race/Ethnicity:Certain racial and ethnic groups have a higher prevalence of autoimmune disorders.
- Environmental factors:Exposure to certain environmental triggers, such as infections, toxins, or stress, can contribute to the development of autoimmune reactions.
- Medical history:Individuals with a history of autoimmune reactions to other vaccines or medications may be at higher risk.
Who Should Consult a Healthcare Professional
Individuals with any of the following risk factors should consult with their healthcare professional before receiving the COVID-19 vaccine:
- A history of autoimmune disorders
- A family history of autoimmune disorders
- A history of autoimmune reactions to other vaccines or medications
- Concerns about potential autoimmune reactions
Managing Autoimmune Reactions After Vaccination
While rare, autoimmune reactions can occur after COVID-19 vaccination. Recognizing and managing these reactions is crucial for patient well-being. This section explores the symptoms, diagnosis, and treatment options for autoimmune reactions triggered by vaccines.
Symptoms and Signs of Autoimmune Reactions
Identifying potential autoimmune reactions after vaccination is essential for prompt medical intervention. The following symptoms and signs may indicate an autoimmune reaction:
- Skin rashes: Red, itchy, or blistering rashes can appear on the skin, sometimes accompanied by swelling.
- Joint pain and swelling: Inflammation of the joints can cause pain, stiffness, and swelling, particularly in the hands, wrists, and knees.
- Muscle aches and fatigue: Persistent muscle pain and unexplained fatigue can be indicative of an autoimmune reaction.
- Neurological symptoms: Autoimmune reactions can affect the nervous system, leading to symptoms such as numbness, tingling, weakness, or even seizures.
- Gastrointestinal issues: Abdominal pain, diarrhea, or nausea can be associated with autoimmune reactions affecting the digestive system.
- Respiratory problems: In some cases, autoimmune reactions can cause shortness of breath, coughing, or chest pain.
Diagnosing Autoimmune Reactions
Diagnosing autoimmune reactions after vaccination requires a thorough medical evaluation. The process typically involves:
- Medical history and physical exam: A detailed review of the patient’s medical history, including previous autoimmune conditions, and a comprehensive physical exam are crucial.
- Blood tests: Blood tests can help detect elevated levels of autoantibodies, which are antibodies that attack the body’s own tissues. Specific blood tests may be ordered depending on the suspected autoimmune condition.
- Imaging studies: Imaging tests, such as X-rays, MRIs, or ultrasounds, may be used to assess inflammation or damage in affected organs.
- Other diagnostic tests: Depending on the specific symptoms, other diagnostic tests, such as nerve conduction studies or biopsies, may be necessary.
Treatment Options for Autoimmune Reactions
Managing autoimmune reactions triggered by vaccines typically involves a multidisciplinary approach. Treatment options may include:
- Immunosuppressive medications: These medications help suppress the immune system to reduce inflammation and prevent further damage to the body’s tissues. Examples include corticosteroids, methotrexate, and azathioprine.
- Biologic therapies: Biologic therapies target specific components of the immune system, helping to reduce inflammation and control autoimmune reactions. Examples include TNF-alpha inhibitors and interleukin-6 inhibitors.
- Plasmapheresis: This procedure removes antibodies from the blood, which can help reduce inflammation and improve symptoms in some cases.
- Supportive care: In addition to medications, supportive care measures, such as rest, pain management, and physical therapy, may be necessary to manage symptoms and improve quality of life.
The Benefits of COVID-19 Vaccination: Why The Body Attacks Itself After Covid 19 Vaccination
The COVID-19 pandemic has had a profound impact on our lives, and vaccination remains a crucial tool in mitigating its effects. While some individuals may experience side effects after receiving the COVID-19 vaccine, the benefits of vaccination far outweigh the risks.
Vaccination against COVID-19 offers numerous advantages, including protection from severe illness, hospitalization, and death. The vaccines work by training the body’s immune system to recognize and fight off the virus, reducing the severity of infection and the risk of complications.
Protection from Severe Illness and Death
COVID-19 vaccination significantly reduces the risk of severe illness and death from the virus. Studies have consistently shown that vaccinated individuals are much less likely to experience severe COVID-19 symptoms, such as pneumonia, respiratory failure, and multi-organ dysfunction. This is particularly important for vulnerable populations, including older adults and individuals with underlying health conditions, who are at higher risk of complications from COVID-19.
A study published in the New England Journal of Medicine found that COVID-19 vaccination reduced the risk of hospitalization and death by 94% among healthcare workers.
The Importance of Weighing Risks and Benefits
Like any medical intervention, COVID-19 vaccination carries a small risk of side effects. However, it is essential to weigh these potential risks against the benefits of protection from severe illness and death. The vast majority of individuals experience mild and temporary side effects, such as pain at the injection site, fatigue, and headache.
These side effects are typically short-lived and do not pose a significant threat to health.
The Centers for Disease Control and Prevention (CDC) has stated that the benefits of COVID-19 vaccination far outweigh the risks for the vast majority of individuals.
Informed Consent and Communication
Informed consent is a fundamental principle in healthcare, and it is essential for individuals to understand the risks and benefits of COVID-19 vaccination before making a decision. Open communication between patients and healthcare providers is crucial in facilitating informed decision-making.
Healthcare professionals should provide patients with accurate and comprehensive information about the vaccine, including its efficacy, safety, and potential side effects. Patients should be encouraged to ask questions and voice their concerns, ensuring they feel comfortable and confident in their decision.
Future Research Directions
While significant progress has been made in understanding the link between COVID-19 vaccination and autoimmune reactions, there are still many unanswered questions. Ongoing research is crucial to address these gaps in knowledge and improve the safety and efficacy of vaccines for all individuals.
Investigating the Mechanisms of Autoimmune Reactions
Understanding the precise mechanisms by which COVID-19 vaccination triggers autoimmune reactions is essential for developing targeted prevention and treatment strategies.
- Immunological Profiling:Comprehensive studies are needed to characterize the specific immune cells, cytokines, and antibodies involved in autoimmune reactions following vaccination. This could involve analyzing blood samples from individuals who develop these reactions, comparing them to those who do not.
- Genetic Susceptibility:Research should investigate the role of genetic factors in predisposing individuals to autoimmune reactions after vaccination. This could involve large-scale genome-wide association studies (GWAS) to identify specific genes associated with an increased risk.
- Molecular Mimicry:Studies exploring the potential for molecular mimicry between viral proteins and self-antigens are crucial. This could involve analyzing the similarities between viral epitopes and human proteins, identifying potential targets for immune responses that could cross-react with self-tissues.
Developing Strategies for Early Detection and Management
Early detection and effective management of autoimmune reactions are critical for minimizing long-term health consequences.
- Biomarker Identification:Research should focus on identifying reliable biomarkers that can predict the development of autoimmune reactions following vaccination. This could involve studying specific blood or tissue markers that indicate an increased risk or early signs of immune dysregulation.
- Therapeutic Interventions:Clinical trials are needed to evaluate the efficacy of different therapeutic interventions for managing autoimmune reactions after vaccination. This could include investigating the use of immunosuppressants, immunomodulators, or other targeted therapies tailored to the specific type of reaction.
- Personalized Medicine:Research should explore the potential for personalized medicine approaches to manage autoimmune reactions. This could involve tailoring treatment strategies based on an individual’s genetic profile, immune status, and the specific type of reaction they experience.
Long-Term Surveillance and Data Collection
Ongoing surveillance and data collection are essential for monitoring the safety and effectiveness of COVID-19 vaccines in the long term.
- Post-Vaccination Surveillance Systems:Robust surveillance systems are needed to track the incidence and severity of autoimmune reactions following vaccination over time. This could involve collecting data from healthcare providers, vaccine registries, and electronic health records.
- Large-Scale Cohort Studies:Large-scale cohort studies that follow vaccinated individuals over extended periods are crucial for assessing the long-term impact of vaccination on autoimmune disease development. This could involve monitoring for the emergence of new autoimmune conditions or changes in existing conditions.
- Data Sharing and Collaboration:Collaboration and data sharing between researchers, healthcare providers, and regulatory agencies are essential for pooling information and gaining a comprehensive understanding of the long-term safety and effectiveness of vaccines.
Ending Remarks
Navigating the complexities of autoimmune reactions after COVID-19 vaccination requires a balanced approach. While the potential for these reactions exists, it’s important to remember that the benefits of vaccination far outweigh the risks for most individuals. Staying informed, consulting with healthcare professionals, and advocating for continued research are crucial steps in ensuring the safety and effectiveness of vaccines for everyone.






