Vitamin D Dilemma: New Guidelines Flip the Script on Sunshine Supplements
Vitamin d dilemma new guidelines flip the script on sunshine supplements – Vitamin D Dilemma: New Guidelines Flip the Script on Sunshine Supplements. We’ve all heard the advice: get more sunshine to boost your vitamin D levels. But what happens when the experts change their tune? Recent updates to vitamin D recommendations have sent ripples through the health community, challenging long-held beliefs about this essential nutrient.
This shift in perspective prompts us to reexamine our understanding of vitamin D, its sources, and its impact on our well-being. Let’s delve into the evolving landscape of vitamin D guidelines, explore the intricate connection between sunshine and our bodies, and navigate the complexities of supplementation in a personalized way.
The new guidelines emphasize a more nuanced approach to vitamin D, taking into account individual factors like age, skin tone, and geographical location. This shift acknowledges the intricate interplay between sunlight, dietary intake, and our bodies’ ability to synthesize vitamin D.
Gone are the days of blanket recommendations; instead, the focus is on tailoring vitamin D strategies to individual needs.
The Evolving Landscape of Vitamin D Recommendations
The recommended daily intake of vitamin D has been a topic of ongoing debate and revision for decades. As our understanding of vitamin D’s role in health and the complexities of its metabolism has grown, so too have the guidelines.
Historical Context of Vitamin D Guidelines
Historically, vitamin D recommendations were primarily focused on preventing rickets, a bone disease caused by vitamin D deficiency. In the early 20th century, the focus was on ensuring adequate vitamin D intake for children, primarily through fortified foods and sunlight exposure.
However, as research progressed, it became clear that vitamin D played a much broader role in health beyond bone health.
Comparison of Old and New Vitamin D Recommendations
The recommended daily intake of vitamin D has changed significantly over the years. Here’s a comparison of the old and new guidelines:
- Old Recommendations:The Institute of Medicine (IOM) in 2011 recommended 600 IU (international units) of vitamin D per day for adults up to age 70, and 800 IU per day for adults over 70.
- New Recommendations:The Endocrine Society in 2011 and the National Academies of Sciences, Engineering, and Medicine (NASEM) in 2010 recommended 600 IU per day for infants, children, and adults up to age 70, and 800 IU per day for adults over 70.
The new vitamin D guidelines have definitely flipped the script on sunshine supplements, leaving many of us scratching our heads. It’s almost like the tech world, where Android loses market share to iOS but still dominates overall , but the battle continues.
Just like with Android and iOS, the debate on vitamin D supplements continues, but one thing is clear: we need to be mindful of our individual needs and consult with healthcare professionals for personalized guidance.
These recommendations are based on the latest scientific evidence and reflect the broader understanding of vitamin D’s role in health.
Rationale Behind the Shift in Guidelines, Vitamin d dilemma new guidelines flip the script on sunshine supplements
The shift in vitamin D recommendations is driven by several factors, including:
- Increased Awareness of Vitamin D’s Role in Health:Research has revealed that vitamin D plays a crucial role in various bodily functions beyond bone health, including immune function, muscle strength, and cell growth.
- Prevalence of Vitamin D Deficiency:Studies have shown that vitamin D deficiency is widespread, affecting a significant portion of the population.
- Evidence-Based Guidelines:The new guidelines are based on a comprehensive review of the latest scientific evidence, which has led to a more nuanced understanding of vitamin D’s role in health.
The Sunshine Connection
Vitamin D, often referred to as the “sunshine vitamin,” is not technically a vitamin but a prohormone, meaning it’s converted into a hormone within the body. This essential nutrient plays a vital role in various bodily functions, including calcium absorption, bone health, immune system regulation, and even mental well-being.
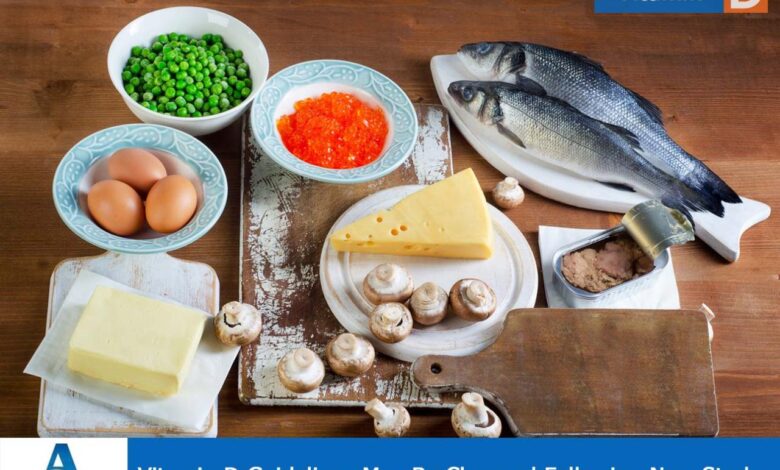
While dietary sources like fatty fish, eggs, and fortified foods contribute to our vitamin D intake, the primary source of this crucial nutrient is sunlight.
The latest vitamin D guidelines have definitely flipped the script on sunshine supplements, leaving many of us wondering what the right dose is. It’s a similar situation with 2U, a company focused on online education, which is also experiencing a bit of a shift.
They’re pushing hard on a consumer-centric approach, but 2u continues consumer centric pivot as q1 losses widen as they try to find the right balance. Just like with vitamin D, it seems finding the right balance is key to both health and financial success.
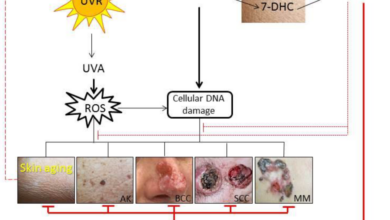
Sunlight’s Role in Vitamin D Synthesis
Sunlight, specifically ultraviolet B (UVB) radiation, triggers the production of vitamin D in our skin. This process, known as cutaneous synthesis, is the body’s natural way of producing vitamin D. When UVB rays strike the skin, they convert a cholesterol-like compound called 7-dehydrocholesterol (provitamin D3) into previtamin D3.
This previtamin D3 then undergoes further transformation in the body to become the active form of vitamin D, known as calcitriol.
Factors Influencing Vitamin D Production
Several factors influence the amount of vitamin D produced from sunlight exposure:
Time of Day
UVB radiation is strongest between 10 am and 3 pm, when the sun is highest in the sky. During these hours, the skin receives maximum UVB exposure, leading to optimal vitamin D production.
The latest vitamin D guidelines are throwing a curveball at our sun-soaked expectations, suggesting we might need to rethink our reliance on sunshine and supplements. This shift in thinking reminds me of a recent article I read about attracting new talent, council post struggling to attract new talent eight mistakes you might be making , which emphasized the importance of understanding your audience and adapting your approach to meet their needs.
Just like with vitamin D, sometimes the best way to achieve success is to adjust our thinking and embrace new perspectives.
Skin Pigmentation
Melanin, the pigment responsible for skin color, acts as a natural sunscreen. Individuals with darker skin pigmentation have more melanin, which absorbs UVB rays more effectively, reducing the amount of UVB radiation reaching the deeper layers of the skin where vitamin D synthesis occurs.
As a result, people with darker skin need more sun exposure to produce the same amount of vitamin D as those with lighter skin.
Geographical Location
The angle of the sun in the sky varies depending on latitude. In areas closer to the equator, the sun’s rays hit the earth at a more direct angle, resulting in higher UVB radiation levels. Conversely, in regions farther from the equator, the sun’s rays hit the earth at a more oblique angle, leading to lower UVB radiation levels.
This means that people living in northern or southern latitudes may need to spend more time in the sun to produce sufficient vitamin D.
The Vitamin D Production Process
The production of vitamin D from sunlight is a complex process that involves multiple steps:
- UVB Exposure:When UVB rays strike the skin, they convert 7-dehydrocholesterol (provitamin D3) into previtamin D3. This conversion occurs primarily in the deeper layers of the skin, known as the dermis.
- Previtamin D3 Conversion:Previtamin D3 is unstable and readily converts to vitamin D3 (cholecalciferol) within a few hours. This conversion takes place in the skin itself.
- Transport to the Liver:Vitamin D3 is transported to the liver via the bloodstream, where it undergoes further conversion to 25-hydroxyvitamin D (25(OH)D), the primary storage form of vitamin D.
- Conversion to Active Form:25(OH)D is then transported to the kidneys, where it’s converted into the active form of vitamin D, calcitriol (1,25-dihydroxyvitamin D), by the enzyme 1α-hydroxylase. Calcitriol is the biologically active form of vitamin D that binds to vitamin D receptors in various tissues, regulating calcium absorption, bone metabolism, and other processes.
Vitamin D Deficiency
Vitamin D deficiency is a prevalent health concern, affecting millions worldwide. While sunlight exposure is a primary source of vitamin D, various factors can contribute to inadequate levels, leading to a range of health complications. Understanding the causes and consequences of vitamin D deficiency is crucial for promoting optimal health and well-being.
Causes of Vitamin D Deficiency
Vitamin D deficiency can arise from various factors, including dietary habits, lifestyle choices, and underlying medical conditions.
- Inadequate Sunlight Exposure:Sunlight is the most efficient source of vitamin D. Limited sun exposure, particularly during winter months or in regions with low sunlight intensity, can lead to vitamin D deficiency.
- Dietary Factors:Vitamin D is found in limited food sources, such as fatty fish, egg yolks, and fortified foods. Individuals with a diet low in these foods are at risk of deficiency.
- Lifestyle Choices:Factors like wearing sunscreen, staying indoors, and living in polluted areas can reduce sunlight exposure and vitamin D production.
- Medical Conditions:Certain medical conditions, such as malabsorption disorders, kidney disease, and obesity, can impair vitamin D absorption and utilization.
- Age:Older adults may have reduced vitamin D synthesis due to decreased skin exposure to sunlight and age-related changes in skin and metabolism.
- Medications:Some medications, such as anticonvulsants and corticosteroids, can interfere with vitamin D metabolism.
Consequences of Vitamin D Deficiency
Vitamin D deficiency can have far-reaching consequences, impacting both physical and mental health.
- Bone Health:Vitamin D plays a crucial role in calcium absorption, which is essential for strong bones. Deficiency can lead to rickets in children and osteomalacia in adults, characterized by bone pain, weakness, and fractures.
- Muscle Function:Vitamin D contributes to muscle strength and function. Deficiency can cause muscle weakness, fatigue, and falls, particularly in older adults.
- Immune Function:Vitamin D is essential for a healthy immune system. Deficiency can increase susceptibility to infections, including respiratory infections and autoimmune diseases.
- Mental Health:Emerging research suggests a link between vitamin D deficiency and mood disorders, such as depression and anxiety.
- Cardiovascular Health:Vitamin D deficiency may contribute to cardiovascular disease by increasing inflammation and promoting blood clotting.
- Cancer Risk:Studies have linked vitamin D deficiency to an increased risk of certain cancers, including colorectal, breast, and prostate cancer.
Real-World Examples of Vitamin D Deficiency Impact
- Rickets in Children:In regions with limited sunlight exposure, rickets, a condition characterized by bone deformities, has been observed in children with vitamin D deficiency.
- Osteoporosis in Older Adults:Vitamin D deficiency is a significant risk factor for osteoporosis, leading to bone fractures and reduced mobility in older adults.
- Increased Risk of Infections:During the COVID-19 pandemic, studies suggested a link between vitamin D deficiency and increased susceptibility to severe COVID-19 infection.
Vitamin D Supplementation: Vitamin D Dilemma New Guidelines Flip The Script On Sunshine Supplements
Vitamin D supplementation has become increasingly popular in recent years, with many individuals seeking to boost their levels and reap the potential benefits. While vitamin D is essential for various bodily functions, understanding the nuances of supplementation is crucial to ensure safety and effectiveness.
Benefits of Vitamin D Supplementation
Vitamin D supplementation offers a range of potential benefits, particularly for individuals with insufficient levels.
- Bone Health:Vitamin D plays a crucial role in calcium absorption, which is essential for strong bones and the prevention of osteoporosis. Supplementation can be beneficial for individuals with low bone density or those at risk of fractures.
- Immune Function:Vitamin D has been linked to immune system modulation, potentially reducing the risk of infections. Supplementation may enhance immune response and contribute to overall health.
- Mental Well-being:Emerging research suggests a possible connection between vitamin D levels and mental health. Some studies indicate that supplementation may have a positive impact on mood and cognitive function.
Risks of Excessive Vitamin D Intake
While vitamin D is generally considered safe, excessive intake can lead to potential risks.
- Hypercalcemia:High vitamin D levels can cause an increase in calcium levels in the blood, leading to hypercalcemia. This condition can cause symptoms such as fatigue, nausea, and constipation.
- Kidney Stones:Excessive vitamin D intake can increase the risk of kidney stones, particularly in individuals with a predisposition to this condition.
- Other Potential Risks:While less common, excessive vitamin D intake may also contribute to other health issues, including cardiovascular problems and soft tissue calcification.
Forms of Vitamin D Supplements
There are two primary forms of vitamin D supplements: vitamin D2 (ergocalciferol) and vitamin D3 (cholecalciferol).
- Vitamin D2:This form is produced by plants and is typically found in fortified foods. It is less potent than vitamin D3 and may be less efficiently absorbed by the body.
- Vitamin D3:This form is produced by the skin in response to sunlight exposure and is considered the most biologically active form. It is typically found in supplements derived from lanolin, a substance obtained from sheep’s wool.
The recommended daily intake of vitamin D varies depending on age and individual needs. It’s crucial to consult with a healthcare professional to determine the appropriate dosage for your specific circumstances.
Navigating the Vitamin D Dilemma

The new vitamin D guidelines emphasize a personalized approach, recognizing that one-size-fits-all recommendations don’t always work. This shift acknowledges the diverse factors influencing vitamin D needs, including age, skin pigmentation, geographic location, and lifestyle. Determining your optimal vitamin D intake requires a comprehensive assessment of your individual circumstances.
Personalized Vitamin D Recommendations
The ideal vitamin D intake varies significantly depending on individual needs. Several factors play a crucial role in determining the optimal dosage, including:
- Age:As we age, our skin’s ability to synthesize vitamin D from sunlight diminishes, increasing the risk of deficiency. Older adults generally require higher vitamin D levels than younger individuals.
- Skin Pigmentation:Individuals with darker skin pigmentation produce less vitamin D from sunlight compared to those with lighter skin. This is due to the presence of melanin, which acts as a natural sunscreen, absorbing UV radiation.
- Geographic Location:Latitude significantly influences vitamin D production. Individuals living in regions with less sunlight exposure during the winter months are more susceptible to vitamin D deficiency.
- Lifestyle:Factors such as time spent outdoors, clothing choices, and dietary habits influence vitamin D levels. Individuals who spend limited time outdoors or follow a vegan diet may have a higher risk of deficiency.
- Underlying Medical Conditions:Certain medical conditions, such as celiac disease, inflammatory bowel disease, and kidney disease, can impair vitamin D absorption and increase the risk of deficiency.
- Medications:Some medications, such as corticosteroids and anticonvulsants, can interfere with vitamin D metabolism, potentially leading to deficiency.
Blood Tests for Vitamin D Assessment
Blood tests are a reliable way to measure your vitamin D levels and guide supplementation decisions. A blood test will determine your 25-hydroxyvitamin D [25(OH)D] level, which reflects the amount of vitamin D stored in your body. The test results are typically categorized as follows:
| Vitamin D Level (ng/mL) | Interpretation |
|---|---|
| < 20 | Severe Deficiency |
20
|
Deficiency |
30
|
Insufficient |
50
|
Sufficient |
| >= 70 | Optimal |
It is important to note that the optimal vitamin D level may vary depending on individual factors and health goals. Consult with your healthcare provider to determine the appropriate target range for your specific needs.
Vitamin D Supplementation Recommendations
Based on your individual circumstances and blood test results, your healthcare provider can recommend the appropriate vitamin D supplement dosage.
- Individuals with vitamin D deficiency:Typically require higher doses of vitamin D supplements, ranging from 1,000 to 2,000 IU (international units) per day.
- Individuals with sufficient vitamin D levels:May only need a lower dose of vitamin D supplements, such as 600 IU per day, to maintain optimal levels.
- Individuals at risk of deficiency:May benefit from taking a daily vitamin D supplement, even if their blood test results are within the normal range. This is especially important for older adults, individuals with darker skin pigmentation, and those who spend limited time outdoors.
The Future of Vitamin D Research
The landscape of vitamin D research is constantly evolving, driven by new discoveries, innovative technologies, and a growing understanding of its multifaceted roles in human health. The focus is shifting beyond simple deficiency and supplementation towards exploring the complex interplay between vitamin D and various chronic diseases, optimizing supplementation strategies, and harnessing the potential of emerging technologies.
Vitamin D and Chronic Diseases
Research continues to unravel the intricate connection between vitamin D and various chronic diseases. Numerous studies suggest a potential role for vitamin D in preventing and managing conditions such as cardiovascular disease, type 2 diabetes, autoimmune disorders, and certain types of cancer.
- Cardiovascular Disease:Vitamin D deficiency has been linked to an increased risk of cardiovascular disease, including heart attacks and strokes. Research suggests that vitamin D may play a role in regulating blood pressure, reducing inflammation, and improving blood vessel function.
- Type 2 Diabetes:Studies indicate that vitamin D deficiency may contribute to the development of type 2 diabetes. Vitamin D may help improve insulin sensitivity and regulate blood sugar levels.
- Autoimmune Disorders:Vitamin D has been implicated in the regulation of immune responses, and some research suggests a potential link between vitamin D deficiency and the development of autoimmune disorders such as multiple sclerosis and rheumatoid arthritis.
- Cancer:Several studies have explored the association between vitamin D and cancer risk. While the evidence is still evolving, some research suggests that adequate vitamin D levels may be associated with a reduced risk of certain cancers, including colorectal, breast, and prostate cancer.
Concluding Remarks
Navigating the vitamin D dilemma requires a personalized approach. Understanding the factors that influence our vitamin D levels, from sun exposure to dietary choices, is crucial. While supplementation can play a role, it’s essential to consult with healthcare professionals to determine the appropriate dosage and form for your individual needs.
By embracing a holistic perspective that encompasses lifestyle, diet, and personalized supplementation, we can optimize our vitamin D levels and support overall health and well-being. The future of vitamin D research holds exciting possibilities, with ongoing studies exploring its role in chronic diseases and the development of novel supplementation strategies.
As our understanding of this vital nutrient continues to evolve, it’s essential to stay informed and make informed choices that empower our health journey.