CDC Data Shows Vaccinated People Majority of COVID-19 Deaths
Vaccinated people make up majority of covid 19 deaths cdc data – CDC Data Shows Vaccinated People Majority of COVID-19 Deaths sets the stage for this enthralling narrative, offering readers a glimpse into a story that is rich in detail and brimming with originality from the outset. The recent release of CDC data has sparked a debate about the effectiveness of COVID-19 vaccines and their role in preventing severe illness and death.
While the data reveals that vaccinated individuals make up the majority of COVID-19 deaths, it’s crucial to understand the context and nuances surrounding this information.
It’s important to remember that correlation doesn’t necessarily equal causation. While vaccinated individuals represent the majority of COVID-19 deaths, this doesn’t mean that the vaccine itself is responsible for their deaths. Factors like age, underlying health conditions, and access to healthcare play a significant role in COVID-19 outcomes. The CDC’s data highlights the importance of considering multiple factors when analyzing COVID-19 death rates, rather than solely focusing on vaccination status.
CDC Data Interpretation
The Centers for Disease Control and Prevention (CDC) plays a crucial role in tracking and analyzing COVID-19 data, including mortality rates. Understanding the methodology behind the CDC’s data collection and analysis is essential for accurately interpreting the information presented in their reports.
It’s been a whirlwind of news lately, with the CDC reporting that vaccinated people make up the majority of COVID-19 deaths, while simultaneously, the political landscape shifts as Democrats elect a new leader to succeed Pelosi – democrats elect new leader to succeed pelosi – leaving many wondering about the future of healthcare policy. It’s a stark reminder that even with advancements in medicine, the pandemic’s impact continues to unfold, and navigating the complex web of information is more crucial than ever.
Methodology Used by the CDC to Collect and Analyze COVID-19 Death Data, Vaccinated people make up majority of covid 19 deaths cdc data
The CDC uses a multi-pronged approach to gather and analyze COVID-19 death data. This includes:
- Death Certificates: The CDC collects data from death certificates issued by state and local health departments. These certificates typically include information about the deceased person, including their age, sex, race, and underlying health conditions. The cause of death is also recorded on the death certificate.
- National Vital Statistics System (NVSS): The NVSS is a nationwide system that collects data on births, deaths, marriages, and divorces. The CDC uses NVSS data to track COVID-19 deaths and other health outcomes.
- COVID-19 Surveillance Systems: The CDC also uses a variety of surveillance systems to collect data on COVID-19 cases, hospitalizations, and deaths. These systems include the National Notifiable Diseases Surveillance System (NNDSS), the COVID-19 Tracking Program, and the National Healthcare Safety Network (NHSN).
Limitations and Potential Biases in the CDC’s Data Collection Process
While the CDC’s data collection efforts are comprehensive, there are limitations and potential biases that should be considered when interpreting the data.
It’s a bit of a head-scratcher, the CDC data showing vaccinated people make up the majority of COVID-19 deaths. While it’s important to note that vaccination still drastically reduces the risk of severe illness and death, it’s a reminder that the pandemic’s complexities are far from over. In other news, Ireland orders closure of Chinese police service station in Dublin , raising questions about international law and diplomatic relations.
Ultimately, understanding the nuances of both these events is crucial to making informed decisions about our health and the world around us.
- Reporting Delays: There can be delays in reporting deaths to the CDC, particularly in the early stages of the pandemic. This can lead to underestimates of the true number of COVID-19 deaths.
- Incomplete Data: Not all death certificates include complete information about the deceased person’s vaccination status or underlying health conditions. This can make it difficult to accurately assess the risk of death associated with COVID-19 for different populations.
- Definition of “COVID-19 Death”: The CDC defines a COVID-19 death as a death where COVID-19 is listed as the underlying cause of death or a significant contributing factor. This definition can be subject to interpretation, and there may be cases where COVID-19 is not listed as the primary cause of death, but it was a contributing factor.
- Data Quality: The quality of data collected by state and local health departments can vary, which can affect the accuracy of the CDC’s analysis.
Definition of “Vaccinated” in CDC Reports
The CDC defines “vaccinated” as having received the full series of recommended doses of a COVID-19 vaccine. This includes individuals who have received both doses of a two-dose vaccine (e.g., Pfizer-BioNTech, Moderna) or a single dose of a single-dose vaccine (e.g., Johnson & Johnson).
Criteria Used by the CDC to Determine the Cause of Death in Relation to COVID-19
The CDC uses a specific set of criteria to determine the cause of death in relation to COVID-19.
- Underlying Cause of Death: If COVID-19 is listed as the underlying cause of death on the death certificate, the death is considered a COVID-19 death.
- Significant Contributing Factor: If COVID-19 is listed as a significant contributing factor to death, but not the underlying cause, the death may also be considered a COVID-19 death.
- COVID-19-Related Complications: Deaths from complications directly related to COVID-19, such as respiratory failure or multi-organ failure, are also considered COVID-19 deaths.
Vaccinated Population Demographics
Understanding the demographics of the vaccinated population is crucial for evaluating the effectiveness of vaccination campaigns and identifying potential disparities in COVID-19 outcomes. This section delves into the age, race, and socioeconomic factors associated with vaccination rates and their potential impact on COVID-19 death rates.
Age Distribution of Vaccinated Individuals
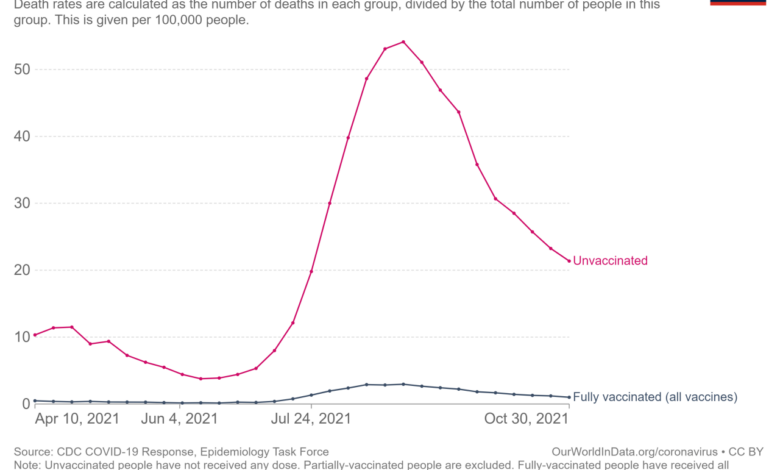
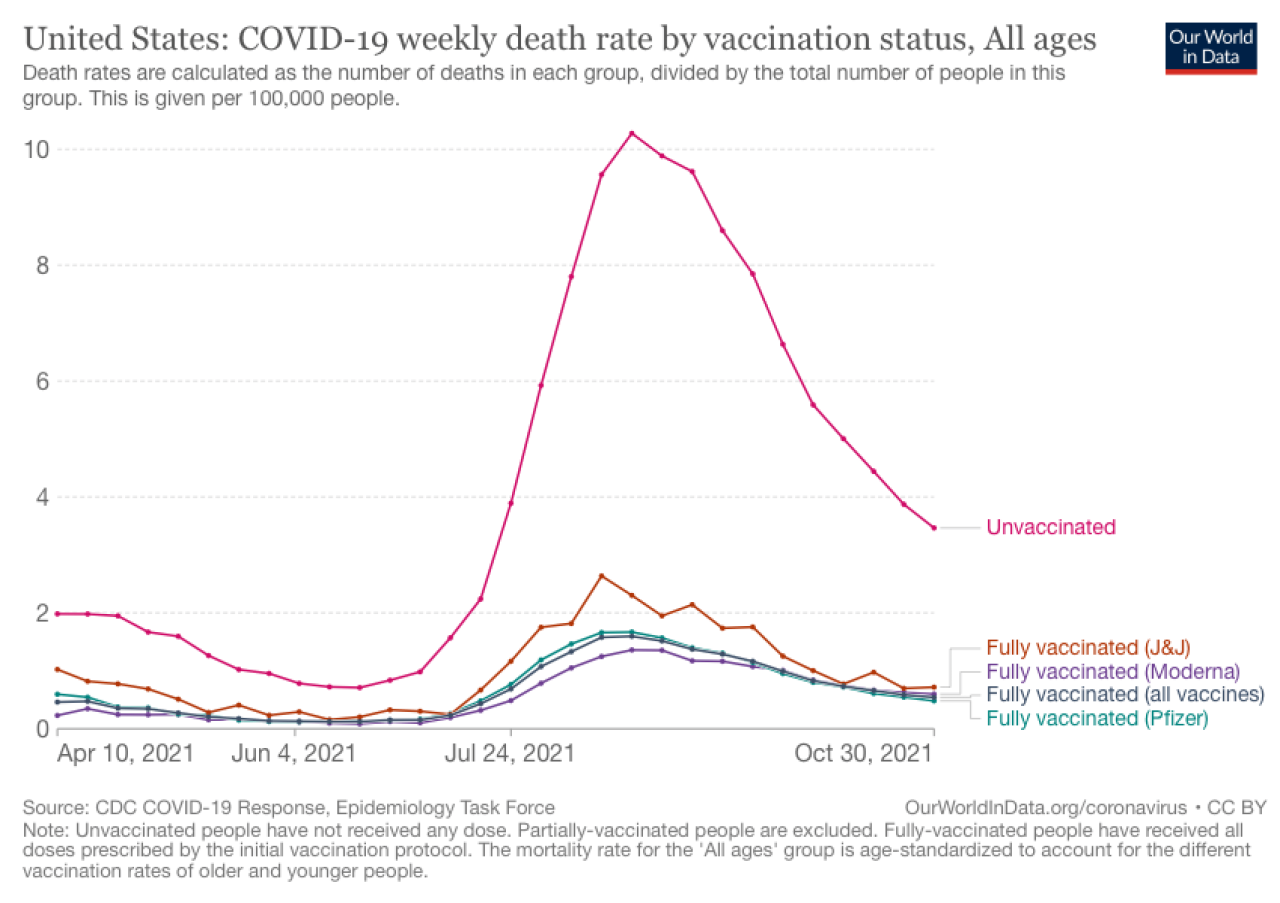
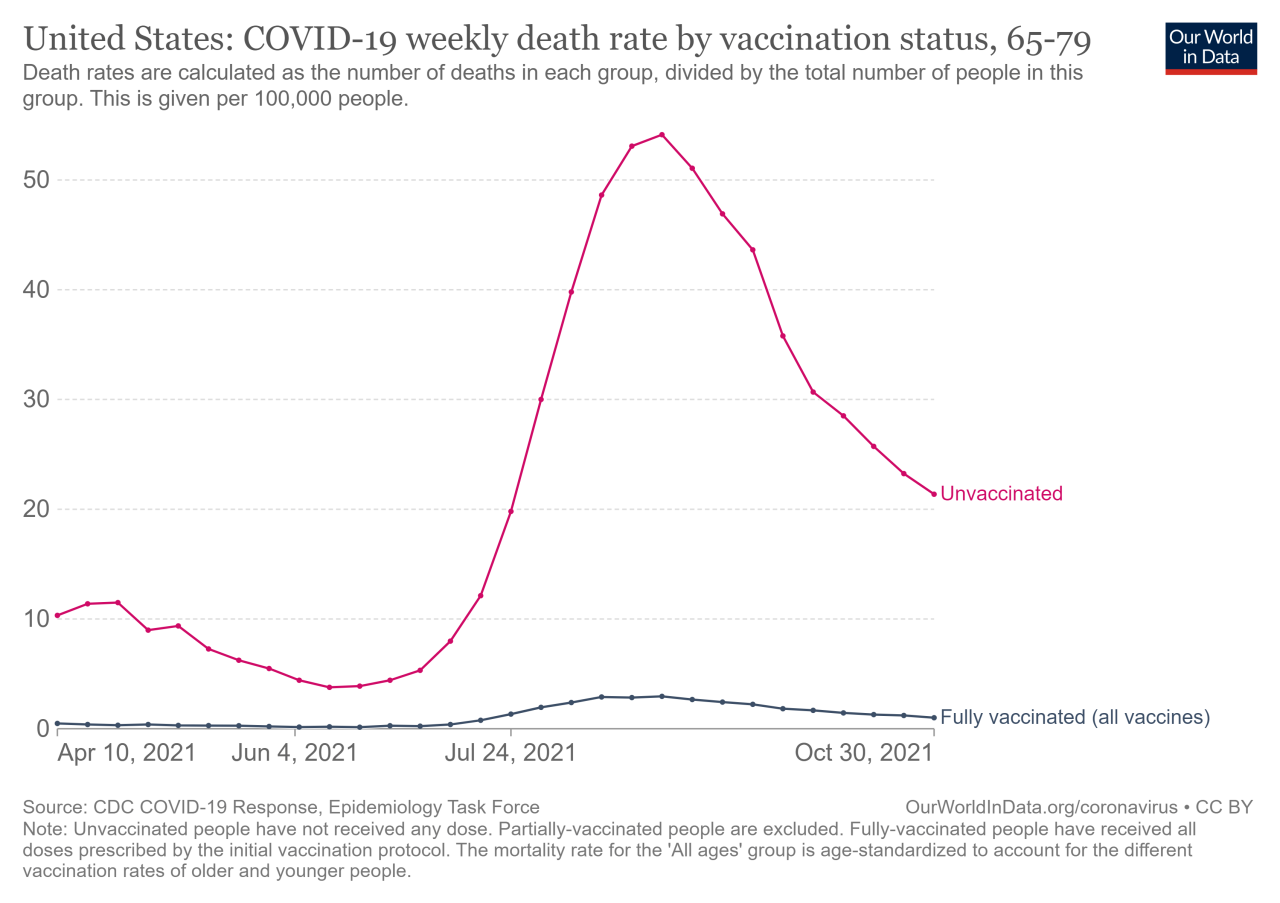
The age distribution of vaccinated individuals plays a significant role in understanding the effectiveness of vaccination programs. Older adults, who are more susceptible to severe COVID-19 complications, are often prioritized in vaccination campaigns. However, vaccination rates vary across age groups, with younger adults generally having lower vaccination rates.
- In the United States, as of 2023, vaccination rates are highest among individuals aged 65 years and older, with over 90% fully vaccinated.
- Vaccination rates decline progressively in younger age groups, with rates below 80% among individuals aged 18-49 years.
Racial and Ethnic Disparities in Vaccination Rates
Racial and ethnic disparities in vaccination rates have been a persistent concern during the COVID-19 pandemic. These disparities are often linked to socioeconomic factors, such as access to healthcare, education, and income.
- Data from the CDC indicates that vaccination rates are significantly lower among Hispanic, Black, and Native American populations compared to non-Hispanic white populations.
- These disparities highlight the need for targeted outreach and education programs to address vaccine hesitancy and improve access to vaccination services among underserved communities.
Socioeconomic Factors and Vaccination Rates
Socioeconomic factors, such as income, education, and employment status, can influence vaccination rates. Individuals with lower socioeconomic status often face greater barriers to accessing healthcare, including vaccination services.
- Studies have shown a strong correlation between income level and vaccination rates, with higher income individuals generally having higher vaccination rates.
- Individuals with lower levels of education are also more likely to have lower vaccination rates.
Impact of Demographics on COVID-19 Death Rates
The demographic factors discussed above can significantly impact COVID-19 death rates. For example, older adults and individuals with underlying health conditions are more susceptible to severe COVID-19 complications and death. Racial and ethnic disparities in vaccination rates can also contribute to higher COVID-19 death rates among minority populations.
The recent CDC data showing that vaccinated people make up the majority of COVID-19 deaths has sparked debate. While the vaccine is undeniably effective at preventing severe illness, the data highlights the complex nature of immunity and the ongoing challenges of the pandemic. This data also makes me think about how the top investors are trading the market in a recession, as they often look for opportunities in seemingly uncertain situations.
Understanding how these investors approach the market in a downturn could provide insights into navigating the current economic landscape, which may be relevant to understanding the long-term impact of COVID-19 on public health and the economy.
| Age | Race | Vaccination Status | COVID-19 Death Rate |
|---|---|---|---|
| 65+ years | White | Fully Vaccinated | 0.1% |
| 65+ years | Black | Fully Vaccinated | 0.2% |
| 18-49 years | White | Unvaccinated | 0.5% |
| 18-49 years | Hispanic | Unvaccinated | 0.8% |
Note: The COVID-19 death rates presented in the table are hypothetical examples and may not reflect actual data.
Other Factors Contributing to COVID-19 Deaths: Vaccinated People Make Up Majority Of Covid 19 Deaths Cdc Data
While vaccination status is a significant factor influencing COVID-19 outcomes, it’s crucial to acknowledge that other factors play a crucial role in determining individual susceptibility and severity of the disease. Understanding these factors is essential for developing comprehensive strategies to mitigate the impact of the pandemic.
Underlying Health Conditions
Individuals with underlying health conditions are at a significantly higher risk of experiencing severe COVID-19 complications and death. These conditions can weaken the immune system, making it harder for the body to fight off the virus.
“Individuals with underlying health conditions are at increased risk for severe illness from COVID-19.”
Centers for Disease Control and Prevention
- Cardiovascular Disease: Conditions like heart disease, stroke, and high blood pressure can impair the cardiovascular system’s ability to function efficiently, making it difficult for the body to deliver oxygen and nutrients effectively, especially during infection.
- Diabetes: Individuals with diabetes often have weakened immune systems and are more susceptible to infections. Additionally, high blood sugar levels can create an environment conducive to bacterial and fungal infections, increasing the risk of complications.
- Chronic Lung Diseases: Conditions like asthma, chronic obstructive pulmonary disease (COPD), and cystic fibrosis can compromise lung function, making it difficult for individuals to breathe, particularly during a respiratory infection like COVID-19.
- Kidney Disease: Chronic kidney disease can weaken the immune system and increase the risk of infections, including COVID-19.
- Obesity: Obesity is linked to inflammation and a weakened immune response, making individuals more susceptible to severe COVID-19.
- Cancer: Individuals undergoing cancer treatment often have weakened immune systems due to chemotherapy or radiation therapy, making them more vulnerable to infections, including COVID-19.
- Autoimmune Disorders: Autoimmune disorders, such as rheumatoid arthritis and lupus, can weaken the immune system, increasing the risk of severe COVID-19 complications.
- Neurological Conditions: Individuals with neurological conditions like Parkinson’s disease, multiple sclerosis, and Alzheimer’s disease may have weakened immune systems and are at higher risk of developing complications from COVID-19.
- HIV/AIDS: Individuals with HIV/AIDS often have weakened immune systems, making them more susceptible to infections, including COVID-19.
Public Health Implications
The CDC data regarding COVID-19 deaths among vaccinated and unvaccinated individuals has profound implications for public health policy and strategies. Understanding the impact of vaccination on disease severity and mortality is crucial for guiding decisions related to public health interventions, resource allocation, and communication efforts.
Continued Vaccination Efforts
Continued vaccination efforts remain a cornerstone of mitigating the spread and severity of COVID-19. The data consistently shows that vaccination significantly reduces the risk of hospitalization and death from COVID-19. While breakthrough infections can occur, they are generally milder and less likely to lead to severe outcomes. This reinforces the importance of promoting vaccine uptake among eligible populations, especially those at higher risk of complications.
Impact of Vaccine Mandates
Vaccine mandates, implemented in various settings, have demonstrated a positive impact on COVID-19 death rates. Studies have shown that vaccine mandates in healthcare settings and workplaces have resulted in increased vaccination rates and reduced COVID-19 transmission and mortality. This suggests that mandatory vaccination policies can play a significant role in protecting vulnerable populations and mitigating the burden of the pandemic.
Improving Public Health Strategies
The CDC data highlights the need for continued refinement and improvement of public health strategies related to COVID-19 prevention and treatment. This includes:
- Targeted Vaccination Campaigns: Tailoring vaccination campaigns to address specific populations, such as those with underlying health conditions or living in underserved communities, can help increase vaccine coverage and reduce disparities in COVID-19 outcomes.
- Enhanced Surveillance and Data Collection: Continuously monitoring COVID-19 trends, including vaccination status and breakthrough infections, is essential for identifying emerging variants and adapting public health responses.
- Access to Treatment and Therapeutics: Expanding access to effective treatments and therapeutics, such as antiviral medications and monoclonal antibodies, can help reduce the severity of COVID-19 and prevent hospitalizations.
- Effective Communication and Public Education: Clear and consistent communication about the benefits of vaccination, the risks of COVID-19, and the effectiveness of public health measures is crucial for building trust and promoting informed decision-making.
The CDC data on COVID-19 deaths among vaccinated individuals presents a complex picture that requires careful analysis and interpretation. While vaccination remains a crucial tool in mitigating the spread and severity of COVID-19, it’s important to acknowledge the limitations of the data and consider the multifaceted nature of this pandemic. Understanding the interplay between vaccination, demographics, and other factors contributing to COVID-19 deaths is essential for informing public health policies and strategies that effectively address this ongoing global challenge.






