Timeline: COVID-19 Vaccines and Myocarditis
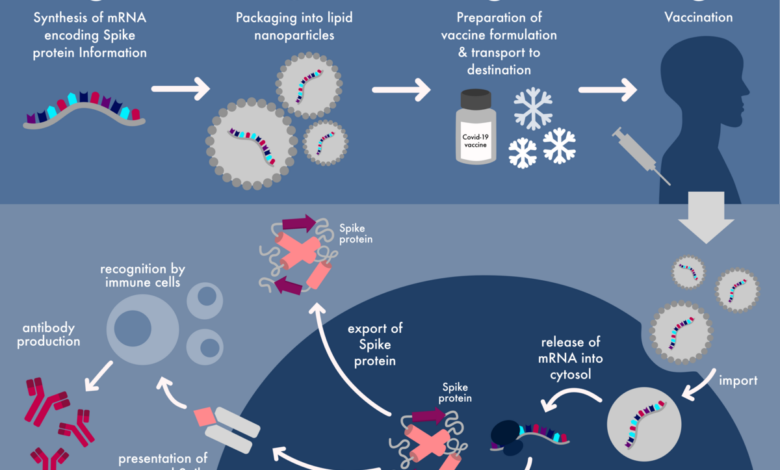
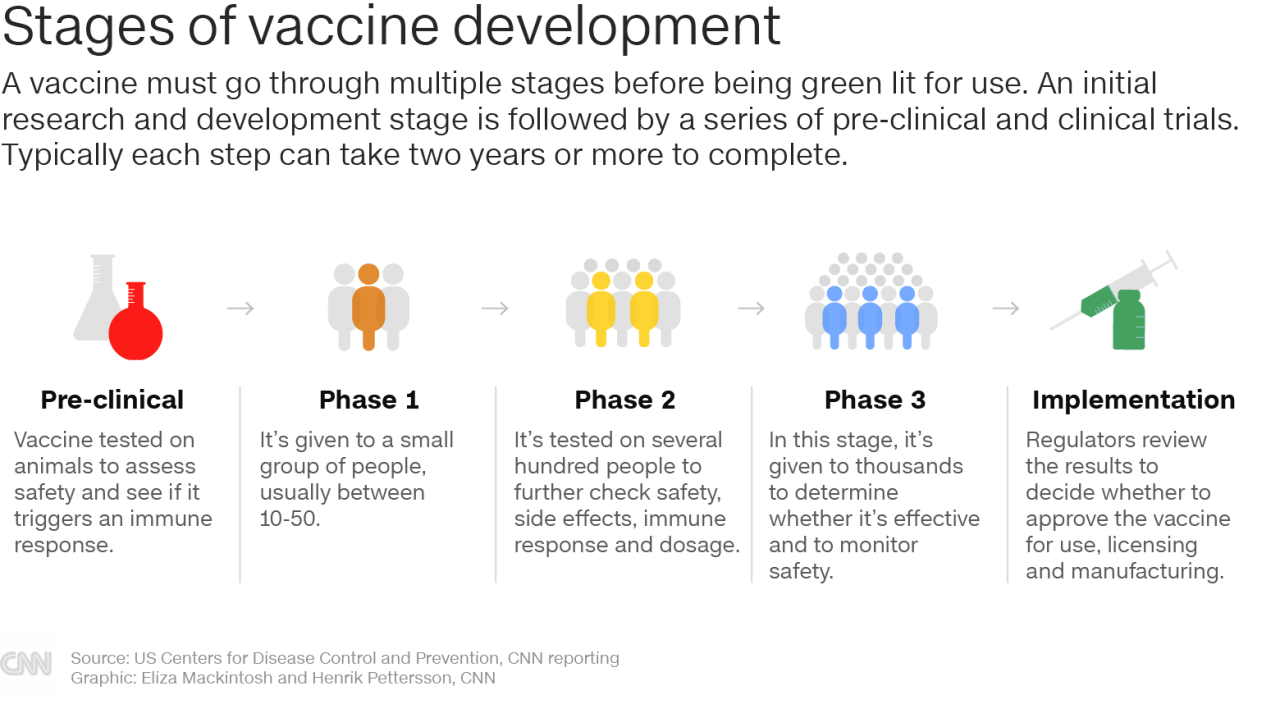
Timeline covid 19 vaccines and myocarditis – Timeline: COVID-19 Vaccines and Myocarditis sets the stage for this enthralling narrative, offering readers a glimpse into a story that is rich in detail and brimming with originality from the outset. The COVID-19 pandemic spurred a rapid development of vaccines, which were crucial in combating the virus.
However, the emergence of myocarditis, a rare but serious inflammation of the heart muscle, in some individuals following vaccination, raised concerns. This blog delves into the timeline of COVID-19 vaccine development and approval, explores the connection between these vaccines and myocarditis, and examines the scientific research, public health recommendations, and the risk-benefit analysis surrounding this issue.
From the initial research and clinical trials to the approval process, we’ll uncover the key milestones that led to the development of these life-saving vaccines. We’ll also delve into the scientific evidence linking COVID-19 vaccines to myocarditis, discuss the observed cases, risk factors, and potential mechanisms involved.
The blog explores the symptoms, treatment options, and the comparison of myocarditis risk from vaccination versus COVID-19 infection. Additionally, we’ll examine the recommendations and guidelines issued by health authorities, the importance of ongoing monitoring, and the critical risk-benefit analysis that individuals need to consider when making vaccination decisions.
Myocarditis and COVID-19 Vaccines
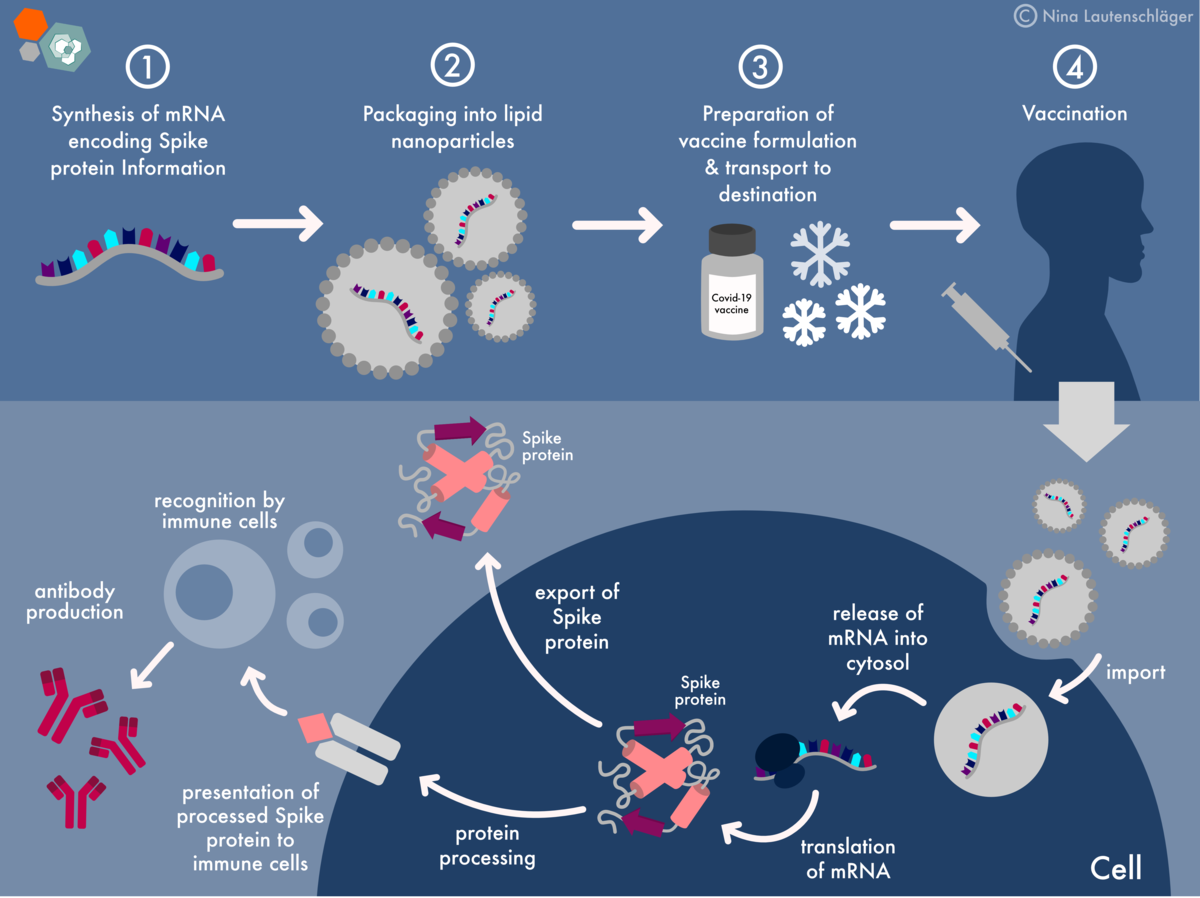
Myocarditis, an inflammation of the heart muscle, has been a topic of discussion in the context of COVID-19 vaccination. While rare, some individuals have experienced myocarditis after receiving certain mRNA vaccines, such as the Pfizer-BioNTech and Moderna vaccines. Understanding the relationship between these vaccines and myocarditis is crucial for informed decision-making.
Observed Cases and Risk Factors
Reports of myocarditis following COVID-19 vaccination have been observed primarily in younger males, particularly adolescents and young adults. The majority of cases have been mild and resolved with treatment. While the exact cause is still being investigated, it is believed that the immune response to the vaccine might play a role.
Risk Factors for Myocarditis
Several factors have been associated with an increased risk of myocarditis after vaccination, including:
- Age:Young males, particularly those under 30, have a higher risk.
- Sex:Males are more likely to experience myocarditis than females.
- Second Dose:The risk of myocarditis is slightly higher after the second dose of the vaccine.
Potential Mechanisms
The exact mechanism by which the vaccines might trigger myocarditis is still being studied. However, current theories suggest that the body’s immune response to the vaccine might inadvertently target the heart muscle, leading to inflammation.
Comparison to COVID-19 Infection
It is important to note that the risk of myocarditis following vaccination is significantly lower than the risk of myocarditis associated with COVID-19 infection. Studies have shown that COVID-19 infection, especially severe cases, can cause myocarditis more frequently and with potentially greater severity than vaccination.
Symptoms and Treatment
Myocarditis after vaccination typically presents with symptoms such as chest pain, shortness of breath, and fatigue. Most cases are mild and resolve within a few days with rest and supportive care. In severe cases, hospitalization and medications, such as anti-inflammatory drugs, may be necessary.
Scientific Research on Myocarditis and Vaccines
Numerous studies have investigated the potential link between COVID-19 vaccines and myocarditis. These studies have employed various methodologies, including observational studies, case-control studies, and large-scale surveillance systems, to examine the occurrence of myocarditis in vaccinated individuals compared to unvaccinated individuals.
The timeline of COVID-19 vaccine development and the potential link to myocarditis has been a subject of intense scrutiny. It’s fascinating to see how the public health landscape shifts, especially when political motivations come into play. Take, for example, the recent news that top Republican orders probe into whether federal funds were used in potential Trump indictment , highlighting the politicization of even the most critical health issues.
While the investigation unfolds, it’s crucial to remember the importance of scientific evidence and objective analysis when evaluating the potential risks and benefits of any medical intervention, particularly those related to public health emergencies.
While the findings from these studies have shed light on the association between COVID-19 vaccines and myocarditis, it’s important to consider the limitations of each study design and the need for further research.
Key Scientific Studies
A comprehensive understanding of the relationship between COVID-19 vaccines and myocarditis requires a review of key scientific studies. These studies provide valuable insights into the potential risks and benefits of vaccination, helping inform public health decisions.
- A study published in the Journal of the American Medical Association (JAMA) in 2021 analyzed data from the Vaccine Adverse Event Reporting System (VAERS) in the United States. The study found a statistically significant increase in reports of myocarditis in young males after receiving mRNA COVID-19 vaccines.
However, the study acknowledged that VAERS is a passive surveillance system, meaning it relies on voluntary reporting, which may not capture all cases of myocarditis.
- Another study, published in the New England Journal of Medicine (NEJM) in 2021, used data from the Israeli Ministry of Health to investigate the risk of myocarditis after mRNA COVID-19 vaccination. The study found an increased risk of myocarditis, particularly in young males, but the risk was generally low.
The study also highlighted the importance of early detection and treatment of myocarditis, as it can be effectively managed with appropriate medical care.
- A large-scale study conducted in the United Kingdom, published in the Lancet in 2022, analyzed data from the UK’s National Health Service (NHS) to assess the risk of myocarditis following mRNA COVID-19 vaccination. The study found a small but statistically significant increased risk of myocarditis, particularly in young males, but the risk was outweighed by the benefits of vaccination.
The study emphasized the need for continued monitoring and further research to understand the long-term effects of myocarditis following vaccination.
Methodologies Used in Studies
The methodologies employed in these studies varied, each with its strengths and limitations.
- Observational studies, such as the JAMA study, rely on collecting data from individuals without manipulating any variables. These studies are useful for identifying associations but cannot establish causality. The limitations of observational studies include potential confounding factors that may influence the observed association between vaccination and myocarditis.
- Case-control studies, such as the NEJM study, compare individuals with myocarditis (cases) to individuals without myocarditis (controls) to identify factors that may be associated with the condition. While case-control studies can help establish causality, they are susceptible to recall bias, where individuals may not accurately remember their exposure to vaccination.
The timeline of COVID-19 vaccine development and the subsequent emergence of concerns regarding myocarditis is a complex story. It’s interesting to see how these events have intersected with legal battles over vaccine mandates, like the recent ruling where a judge ruled that teachers who refused the COVID-19 vaccine can get their jobs back with back pay.
This ruling raises questions about the balance between individual rights and public health concerns, especially as we continue to learn more about the long-term effects of COVID-19 vaccines. The ongoing research on myocarditis and its potential connection to the vaccine remains a crucial area of study.
- Large-scale surveillance systems, such as the UK’s NHS data used in the Lancet study, provide valuable information on the incidence of myocarditis in a large population. These systems can identify trends and associations but may not be able to provide detailed information on individual cases.
Limitations of Findings, Timeline covid 19 vaccines and myocarditis
Despite the valuable insights provided by these studies, it’s crucial to acknowledge the limitations of their findings.
It’s been a wild ride trying to keep up with the timeline of COVID-19 vaccines and their potential side effects. Early on, myocarditis was a major concern, and now we’re hearing about covid boosters triggering metastasis. It’s definitely a lot to process, and it makes me wonder if we’re just starting to see the long-term effects of these vaccines.
- The studies primarily focused on mRNA vaccines, and the findings may not be generalizable to other types of COVID-19 vaccines.
- The studies relied on data from specific populations, such as the United States, Israel, and the United Kingdom, and the findings may not be applicable to other populations with different genetic and environmental factors.
- The studies were limited by the availability and completeness of data, and the findings may not reflect the true incidence of myocarditis following vaccination.
Areas for Further Research
While the available research has provided valuable information, further research is needed to fully understand the relationship between COVID-19 vaccines and myocarditis.
- Long-term studies are needed to assess the long-term effects of myocarditis following vaccination.
- Studies are needed to investigate the mechanisms by which COVID-19 vaccines may trigger myocarditis.
- Studies are needed to determine whether there are specific risk factors for myocarditis following vaccination.
- Studies are needed to develop strategies for preventing and managing myocarditis following vaccination.
Public Health Recommendations and Guidelines
The occurrence of myocarditis, a rare but serious side effect, following COVID-19 vaccination has led to ongoing monitoring and evolving recommendations from public health authorities worldwide. This section will explore the guidelines and recommendations issued by health authorities regarding myocarditis and COVID-19 vaccines, delving into the rationale behind these recommendations and their evolution over time.
The importance of ongoing monitoring and data collection to inform public health decisions will also be discussed.
Recommendations and Guidelines
Health authorities, such as the Centers for Disease Control and Prevention (CDC) and the European Medicines Agency (EMA), have issued recommendations and guidelines regarding myocarditis and COVID-19 vaccines. These guidelines aim to balance the benefits of vaccination against the risks of myocarditis.
- The CDC recommends that individuals who experience chest pain, shortness of breath, or other symptoms suggestive of myocarditis after receiving a COVID-19 vaccine should seek immediate medical attention.
- The EMA has issued guidance for healthcare professionals on the diagnosis and management of myocarditis following COVID-19 vaccination.
- Both the CDC and the EMA emphasize the importance of ongoing monitoring and data collection to better understand the risk of myocarditis following COVID-19 vaccination.
Rationale Behind Recommendations
The recommendations and guidelines regarding myocarditis and COVID-19 vaccines are based on a comprehensive understanding of the available scientific evidence. This evidence includes data from clinical trials, observational studies, and post-marketing surveillance.
- The benefits of COVID-19 vaccination, including protection against severe disease, hospitalization, and death, outweigh the risks of myocarditis, which is a rare event.
- The risk of myocarditis following COVID-19 vaccination is higher in younger males, particularly after the second dose of mRNA vaccines.
- The majority of myocarditis cases reported after COVID-19 vaccination have been mild and resolved with supportive care.
Evolution of Recommendations
The recommendations and guidelines regarding myocarditis and COVID-19 vaccines have evolved over time as more data has become available. This ongoing process of learning and adaptation is crucial for ensuring that public health recommendations are based on the most up-to-date scientific evidence.
- Early recommendations focused on raising awareness of the potential risk of myocarditis following COVID-19 vaccination, particularly in younger males.
- As more data has become available, recommendations have been refined to include information on the characteristics of myocarditis cases, the potential risk factors, and the effectiveness of treatment.
- The recommendations also highlight the importance of ongoing monitoring and data collection to further understand the risk of myocarditis and to identify any potential strategies for mitigation.
Importance of Ongoing Monitoring and Data Collection
Ongoing monitoring and data collection are essential for informing public health decisions regarding myocarditis and COVID-19 vaccines. This data is used to:
- Track the incidence of myocarditis following COVID-19 vaccination.
- Identify potential risk factors for myocarditis.
- Evaluate the effectiveness of different treatments for myocarditis.
- Develop strategies for mitigating the risk of myocarditis.
Risk-Benefit Analysis and Decision-Making: Timeline Covid 19 Vaccines And Myocarditis
Making informed decisions about COVID-19 vaccination requires careful consideration of the potential risks and benefits, especially in light of the association between some vaccines and myocarditis. This analysis is crucial for individuals to weigh the potential benefits of protection against COVID-19 against the potential risks of adverse events, including myocarditis.
Risk-Benefit Assessment in the Context of Myocarditis
The risk-benefit analysis involves comparing the likelihood and severity of potential harms from vaccination with the likelihood and severity of benefits. In the context of myocarditis, the benefits of COVID-19 vaccination generally outweigh the risks for most individuals.
- Benefits of COVID-19 Vaccination:
- Protection against severe COVID-19 illness, hospitalization, and death.
- Reduced risk of long COVID, a condition characterized by persistent symptoms after an initial COVID-19 infection.
- Contribution to herd immunity, protecting vulnerable individuals who cannot be vaccinated.
- Risks of COVID-19 Vaccination:
- Myocarditis:A rare but possible side effect, particularly in younger males after receiving mRNA vaccines. The majority of cases are mild and resolve on their own with treatment.
- Other side effects:Common side effects include pain, redness, and swelling at the injection site, fatigue, headache, and muscle aches. These are generally mild and temporary.
Factors to Consider in Decision-Making
Several factors should be considered when making vaccination decisions, including:
- Personal health history:Individuals with pre-existing heart conditions or other health concerns should consult with their healthcare provider to discuss the risks and benefits of vaccination.
- Risk factors for COVID-19:Individuals with higher risk factors for severe COVID-19 illness, such as older age, underlying health conditions, or weakened immune systems, may benefit more from vaccination.
- Individual risk tolerance:Individuals’ personal views on risk and the severity of potential harms from vaccination should be considered.
- Access to reliable information:Individuals should rely on credible sources of information, such as the Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO), to make informed decisions.
Table of Risks and Benefits
| Risks | Benefits |
|---|---|
| Myocarditis (rare, typically mild) | Protection against severe COVID-19 illness, hospitalization, and death |
| Other side effects (generally mild and temporary) | Reduced risk of long COVID |
| Potential for allergic reaction (rare) | Contribution to herd immunity |
Wrap-Up
Navigating the complexities of vaccine safety and efficacy is crucial in a world grappling with emerging health challenges. This blog aims to shed light on the timeline of COVID-19 vaccine development and the link between these vaccines and myocarditis. It’s important to remember that while myocarditis is a rare side effect, the benefits of vaccination far outweigh the risks for most individuals.
Understanding the science, the recommendations, and the individual risk factors empowers us to make informed decisions about our health and well-being. As we continue to learn more about COVID-19 and its impact, ongoing research and public health vigilance are vital in ensuring the safety and effectiveness of vaccines in the long term.