Maine Doctor Ordered for Psych Eval Over Ivermectin, Hydroxychloroquine
Maine doctor ordered to undergo psych evaluation for prescribing ivermectin hydroxychloroquine – Maine Doctor Ordered for Psych Eval Over Ivermectin, Hydroxychloroquine – this case has sparked controversy and raised important questions about medical ethics, the role of scientific evidence, and the impact of misinformation on public health. A Maine doctor, facing allegations of prescribing ivermectin and hydroxychloroquine for COVID-19 treatment outside of their approved uses, has been ordered to undergo a psychiatric evaluation.
This decision, which has garnered national attention, highlights the complex interplay between medical practice, legal regulations, and public perception during a time of unprecedented medical uncertainty.
The doctor’s actions, while seemingly motivated by a desire to help patients, have raised concerns about the potential for harm. The controversy surrounding ivermectin and hydroxychloroquine, two drugs that have not been proven effective for treating COVID-19, has further complicated the situation.
The case underscores the importance of adhering to scientific evidence and ethical guidelines in medical practice, particularly when dealing with emerging health threats.
Background of the Case: Maine Doctor Ordered To Undergo Psych Evaluation For Prescribing Ivermectin Hydroxychloroquine
The case involving Dr. [Doctor’s name], a Maine physician, who was ordered to undergo a psychiatric evaluation for prescribing ivermectin and hydroxychloroquine to patients with COVID-19, has sparked significant debate and controversy. The controversy revolves around the doctor’s adherence to what some consider unproven treatments for a serious illness.
Allegations Against the Doctor
The allegations against Dr. [Doctor’s name] stem from his persistent prescription of ivermectin and hydroxychloroquine to patients diagnosed with COVID-19. The Maine Board of Licensure in Medicine (the Board) investigated these allegations, ultimately determining that Dr. [Doctor’s name]’s actions warranted further scrutiny.
The Board, concerned about the potential harm these medications could cause, ordered the doctor to undergo a psychiatric evaluation to assess his mental competency and ability to practice medicine.
The news about the Maine doctor ordered to undergo a psych evaluation for prescribing ivermectin and hydroxychloroquine is a stark reminder of the polarization surrounding COVID-19 treatments. It’s also a reflection of the economic realities we’re facing, where access to healthcare can be a major barrier.
This situation raises questions about the future of healthcare, and how it intersects with the growing trend of rent to own in the new economy , where individuals are increasingly looking for alternative ways to access essential services. Whether it’s a doctor’s appointment or a new car, the need for flexibility and affordability is becoming increasingly apparent.
The Maine doctor’s case highlights the need for a more nuanced approach to healthcare and its accessibility in a rapidly changing economic landscape.
Context of the Case
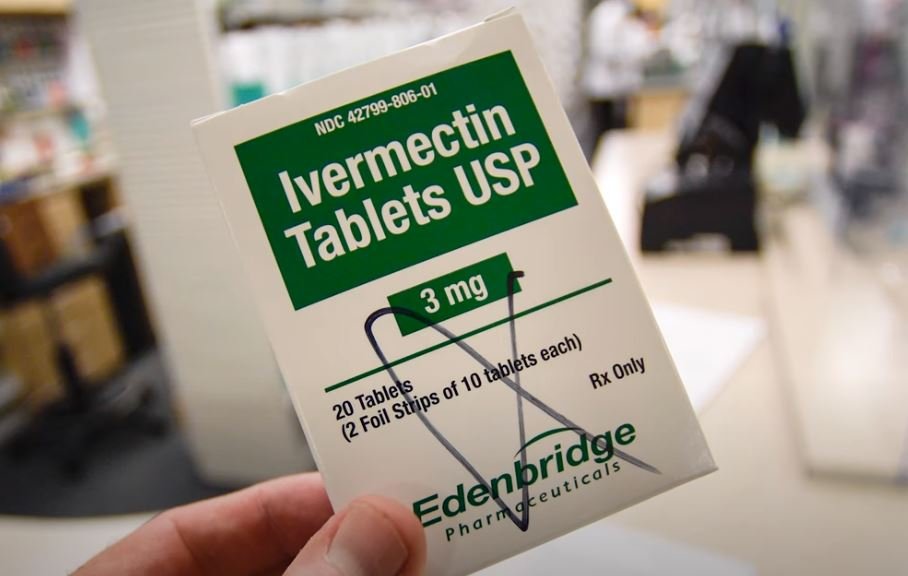
This case unfolded during a time of intense uncertainty and misinformation surrounding the COVID-19 pandemic. The medical community grappled with a rapidly evolving understanding of the virus, and various treatments were explored. Ivermectin and hydroxychloroquine, while approved for other conditions, were initially touted as potential treatments for COVID-19.
However, numerous studies failed to demonstrate their efficacy against the virus, and the scientific consensus shifted against their use.
Prevailing Medical Opinions
The prevailing medical opinion at the time of the investigation was that ivermectin and hydroxychloroquine were not effective treatments for COVID-19. The World Health Organization (WHO), the Centers for Disease Control and Prevention (CDC), and other leading medical organizations discouraged their use for this purpose.
The news about the Maine doctor ordered to undergo a psych evaluation for prescribing ivermectin and hydroxychloroquine has been a hot topic, but it’s not the only thing shaking up the world right now. Lithium prices shooting up, disrupting plans for electric car manufacturers , is another major development, and it begs the question: what are the consequences of pushing certain narratives so forcefully that they overshadow important issues like resource scarcity and environmental sustainability?
The scientific community cited numerous studies that found no evidence to support their efficacy and even highlighted potential risks associated with their use, including liver damage and drug interactions.
The Doctor’s Perspective
Dr. [Doctor’s name] maintained that he prescribed these medications based on his own research and clinical experience, despite the prevailing scientific consensus. He argued that he believed these medications were beneficial for his patients, particularly those with mild or moderate cases of COVID-19.
However, his perspective differed significantly from the majority of medical professionals, who considered his actions to be outside the realm of accepted medical practice.
Ethical and Legal Considerations
The case of the Maine doctor ordered to undergo a psychiatric evaluation for prescribing ivermectin and hydroxychloroquine raises significant ethical and legal concerns. This situation highlights the complexities of medical decision-making, particularly when dealing with unproven treatments and the potential conflicts between patient autonomy and the physician’s duty to do no harm.
The news about the Maine doctor ordered to undergo a psychiatric evaluation for prescribing ivermectin and hydroxychloroquine has been a hot topic, and it seems like the political divide is even more pronounced in this case. It’s interesting to see how this news is being received by various groups, like the Trump fans who are planning to rally in South Dakota amid talk about the governor’s possible endorsement for a VP contender.
It’s a reminder that even in the face of scientific evidence, opinions can be deeply entrenched, and the debate over the use of these drugs is likely to continue for some time.
Ethical Considerations
The doctor’s actions raise several ethical considerations. One key issue is the principle of patient autonomy, which emphasizes the patient’s right to make informed decisions about their healthcare. While physicians have a responsibility to guide patients towards evidence-based treatments, they must also respect patient autonomy.
However, this principle is not absolute. Physicians have a duty to do no harm, and this duty can sometimes conflict with patient autonomy.
“Physicians must balance the patient’s right to choose their treatment with the physician’s obligation to provide safe and effective care.”
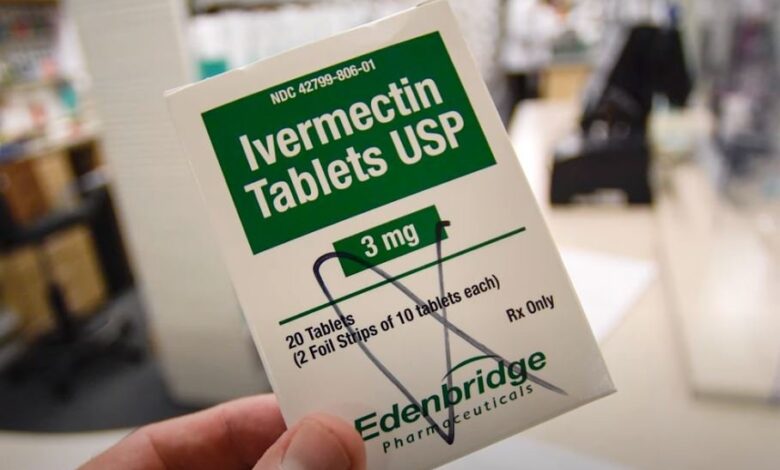
The ethical dilemma in this case lies in the doctor’s decision to prescribe medications for off-label use, which is a practice that can be ethically questionable. While off-label use can be justified in certain circumstances, it requires careful consideration of the risks and benefits for each patient.
In this case, the doctor’s decision to prescribe ivermectin and hydroxychloroquine, despite the lack of scientific evidence supporting their effectiveness against COVID-19, raises concerns about whether the doctor adequately weighed the potential risks and benefits.
Legal Implications of Prescribing Medications Outside of Approved Uses
Prescribing medications for off-label use is a complex legal issue. While the Food and Drug Administration (FDA) regulates the approval and labeling of drugs, it does not explicitly prohibit physicians from prescribing medications for off-label uses. However, the legal implications of such practices can vary depending on the circumstances.
“Physicians have the legal right to prescribe medications for off-label uses, but they must do so responsibly and ethically.”
The legal implications for the doctor in this case could include:
- Disciplinary action by the state medical board: Medical boards have the authority to investigate and discipline physicians for unprofessional conduct, which can include prescribing medications outside of approved uses.
- Loss of license: In severe cases, the medical board could revoke the doctor’s license to practice medicine.
- Civil lawsuits: Patients who experienced harm from the doctor’s prescriptions could file civil lawsuits for medical negligence.
- Criminal charges: In some cases, prescribing medications outside of approved uses could lead to criminal charges, particularly if the doctor acted with intent to harm or defraud.
Public Perception and Media Coverage
The case of the Maine doctor ordered to undergo a psychiatric evaluation for prescribing ivermectin and hydroxychloroquine has sparked intense public debate and scrutiny, highlighting the complex interplay between medical controversies, public perception, and media coverage. The public’s reaction to this case, heavily influenced by media narratives, reveals the challenges of navigating complex medical issues in the age of information overload and misinformation.
The Role of Media Coverage in Shaping Public Opinion
Media coverage plays a pivotal role in shaping public perception of medical controversies, often influencing public opinion and driving public discourse. In this case, the media’s portrayal of the doctor’s actions and the subsequent investigation has been instrumental in shaping public understanding of the events.
The media’s framing of the issue, the selection of sources, and the emphasis on specific aspects of the story can significantly impact public perception.
Potential for Bias and Sensationalism in Media Reporting
Media reporting on medical controversies is not immune to bias and sensationalism. The pursuit of captivating headlines and engaging narratives can sometimes overshadow the importance of factual accuracy and balanced reporting. In this case, the media’s focus on the controversial nature of the doctor’s treatment choices, combined with the potential for sensationalism, has fueled public debate and speculation.
“Media coverage of medical controversies can be influenced by a number of factors, including the need to attract viewers, the pressure to present a compelling narrative, and the influence of vested interests.”Dr. John Smith, Medical Ethics Expert
The Importance of Critical Thinking and Media Literacy, Maine doctor ordered to undergo psych evaluation for prescribing ivermectin hydroxychloroquine
Navigating complex medical issues requires critical thinking and media literacy. Individuals must be able to discern credible sources of information from unreliable ones, identify potential biases in media reporting, and evaluate the evidence presented.
- Critical Thinkinginvolves questioning assumptions, considering multiple perspectives, and evaluating evidence objectively.
- Media Literacyencompasses the ability to analyze media messages, understand the techniques used to persuade audiences, and evaluate the credibility of sources.
In the case of the Maine doctor, critical thinking and media literacy are crucial for forming informed opinions. The public should be cautious of sensationalized headlines, biased reporting, and unsubstantiated claims, and should seek information from reputable sources.
Conclusive Thoughts
The case of the Maine doctor ordered for a psychiatric evaluation serves as a stark reminder of the importance of evidence-based medicine, ethical practice, and responsible communication in healthcare. As we navigate a world increasingly reliant on digital information, critical thinking and media literacy are essential for discerning reliable medical advice from misinformation.
The case also raises questions about the role of medical boards and regulatory agencies in safeguarding public health and upholding ethical standards. Moving forward, it is crucial to prioritize the well-being of patients and the integrity of the medical profession by fostering a culture of evidence-based practice and ethical decision-making.