NHS Doctor Tells UK Health Secretary: I Dont Want to Be Vaccinated
“I do not want to have a vaccination nhs doctor tells uk health secretary” – this bold statement, made by a UK doctor, has sent shockwaves through the country’s healthcare system and ignited a fiery debate about vaccination, trust, and individual autonomy.
The doctor’s declaration, made public amidst a backdrop of ongoing vaccination campaigns and a surge in vaccine hesitancy, has thrown a spotlight on the complex interplay between personal beliefs, medical expertise, and public health policies.
The statement has sparked a flurry of reactions, with many questioning the doctor’s motives and the potential implications for the NHS’s vaccination strategy. This incident raises crucial questions about the role of healthcare professionals in promoting vaccination, the power dynamics between doctors and patients, and the delicate balance between individual choice and collective well-being.
The Context of the Statement

The statement “I do not want to have a vaccination” made by an NHS doctor to the UK Health Secretary is a significant event in the UK healthcare landscape, particularly considering the context of the ongoing COVID-19 pandemic. This statement, while seemingly simple, carries weight due to the doctor’s position within the healthcare system and the implications it holds for public health and trust in healthcare authorities.To understand the significance of this statement, it’s crucial to examine the historical context of vaccination policies and public sentiment towards them in the UK.
Vaccination has been a cornerstone of public health in the UK for centuries, with a long history of successful campaigns against diseases like smallpox, measles, and polio. Public trust in vaccination has generally been high, with high uptake rates for recommended vaccines.
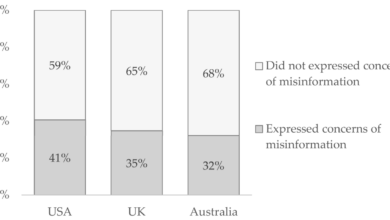
However, this trust has been challenged in recent years due to factors like the emergence of anti-vaccination movements, misinformation, and concerns about vaccine safety.
The Potential Implications of the Statement for Public Health and Trust in Healthcare Authorities
The statement by the NHS doctor could have significant implications for public health and trust in healthcare authorities. It could fuel existing anti-vaccination sentiments, potentially leading to a decline in vaccination uptake rates. This could result in a resurgence of preventable diseases, jeopardizing the progress made in public health over decades.The statement could also erode public trust in healthcare professionals and institutions.
If a doctor, who is expected to be a trusted source of medical information, expresses reluctance towards vaccination, it could raise doubts in the minds of the public about the safety and efficacy of vaccines. This could have far-reaching consequences, making it more difficult to implement future public health initiatives and campaigns.The statement could also have implications for the government’s efforts to combat the COVID-19 pandemic.
The UK has been heavily reliant on vaccination to control the spread of the virus, and any decline in vaccination uptake could undermine these efforts. This could lead to a resurgence of cases, strain on the healthcare system, and potentially necessitate further lockdowns and restrictions.
The Role of the NHS Doctor

The statement made by the NHS doctor, refusing to administer the COVID-19 vaccine, has sparked a heated debate, raising questions about the role and responsibilities of healthcare professionals in a public health crisis. It is essential to analyze the potential motivations behind the doctor’s actions and consider the ethical implications of their public declaration.
It’s fascinating how the focus on individual choices, like the “I do not want to have a vaccination” statement, can sometimes overshadow broader societal issues. The recent reports from Texas law enforcement, revealing the scope of the border crisis , highlight the complex challenges we face as a global community.
It’s a reminder that even as we grapple with personal decisions, we must also acknowledge the interconnectedness of our world and the need for collective action.
Potential Motivations
The doctor’s decision to publicly declare their refusal to vaccinate may stem from a variety of factors. It is crucial to understand the potential motivations to gain a comprehensive perspective on the situation.
It’s becoming increasingly clear that the “I do not want to have a vaccination” sentiment is gaining traction. The NHS doctor’s plea to the UK Health Secretary highlights a growing distrust in the system. Some are even drawing connections to conspiracy theories like bill gates plots a global pandemic prison state , claiming a hidden agenda behind the push for widespread vaccination.
Whether these concerns are justified or not, they underscore the importance of open dialogue and transparency surrounding vaccination policies.
- Personal Beliefs:The doctor might hold strong personal beliefs against vaccination, based on concerns about its safety, efficacy, or ethical implications. These beliefs could be rooted in religious, philosophical, or scientific skepticism.
- Misinformation and Disinformation:The doctor might have been influenced by misinformation or disinformation circulating online and in certain communities, leading to doubts about the vaccine’s safety or necessity. This exposure to misleading information could have swayed their judgment.
- Conspiracy Theories:The doctor might subscribe to conspiracy theories surrounding the vaccine, believing it to be part of a larger agenda to control or harm the population. These theories, often lacking scientific evidence, can create a strong sense of distrust and lead to vaccine hesitancy.
- Lack of Trust in Authorities:The doctor might have lost trust in public health authorities or the government, questioning their motives and the validity of their recommendations. This lack of trust can lead to a rejection of the vaccine, even if they recognize its potential benefits.
- Fear of Side Effects:The doctor might be genuinely concerned about the potential side effects of the vaccine, even though the risks are generally low and outweighed by the benefits. This fear could be amplified by personal experiences or anecdotal accounts of adverse reactions.
Ethical Considerations
A healthcare professional’s decision to publicly declare their refusal to vaccinate raises significant ethical concerns. The ethical principles that guide medical practice, such as beneficence, non-maleficence, autonomy, and justice, are all implicated in this situation.
- Beneficence and Non-maleficence:Healthcare professionals have a duty to act in the best interests of their patients and avoid causing harm. By refusing to vaccinate, the doctor may be putting their patients at risk of contracting and spreading a potentially deadly disease.
The news about the NHS doctor’s statement regarding vaccine hesitancy in the UK is certainly concerning, but it’s interesting to see how the political landscape is also reflecting similar sentiments. For example, Donald Trump’s recent move to request Judge Tanya Chutkan’s recusal in a federal case trump files motion for judge tanya chutkan to recuse herself in federal case highlights a growing distrust in institutions and a desire for individual autonomy, mirroring the anti-vaccine stance expressed by some.
Whether these sentiments are justified or not, they are clearly impacting public discourse and policy decisions.
- Autonomy:While patients have the right to refuse medical treatment, healthcare professionals have a responsibility to provide evidence-based information and guidance to help patients make informed decisions. The doctor’s public declaration may undermine trust in medical professionals and discourage patients from seeking vaccination.
- Justice:The doctor’s refusal to vaccinate could contribute to health disparities and inequities, as vulnerable populations are disproportionately affected by infectious diseases. By refusing to participate in public health efforts, the doctor may be perpetuating existing inequalities.
Potential Consequences
The doctor’s public declaration could have serious consequences for their career and reputation.
- Disciplinary Action:The doctor’s actions may violate professional codes of conduct and could lead to disciplinary action by their employer or regulatory body. This could include suspension, reprimand, or even loss of their medical license.
- Damage to Reputation:The doctor’s public stance against vaccination could damage their reputation within the medical community and among the public. This could lead to a loss of trust and credibility, making it difficult to maintain their practice or secure employment.
- Legal Implications:The doctor’s actions could also have legal implications, particularly if they are found to have acted negligently or in violation of patient care standards. This could result in lawsuits or other legal proceedings.
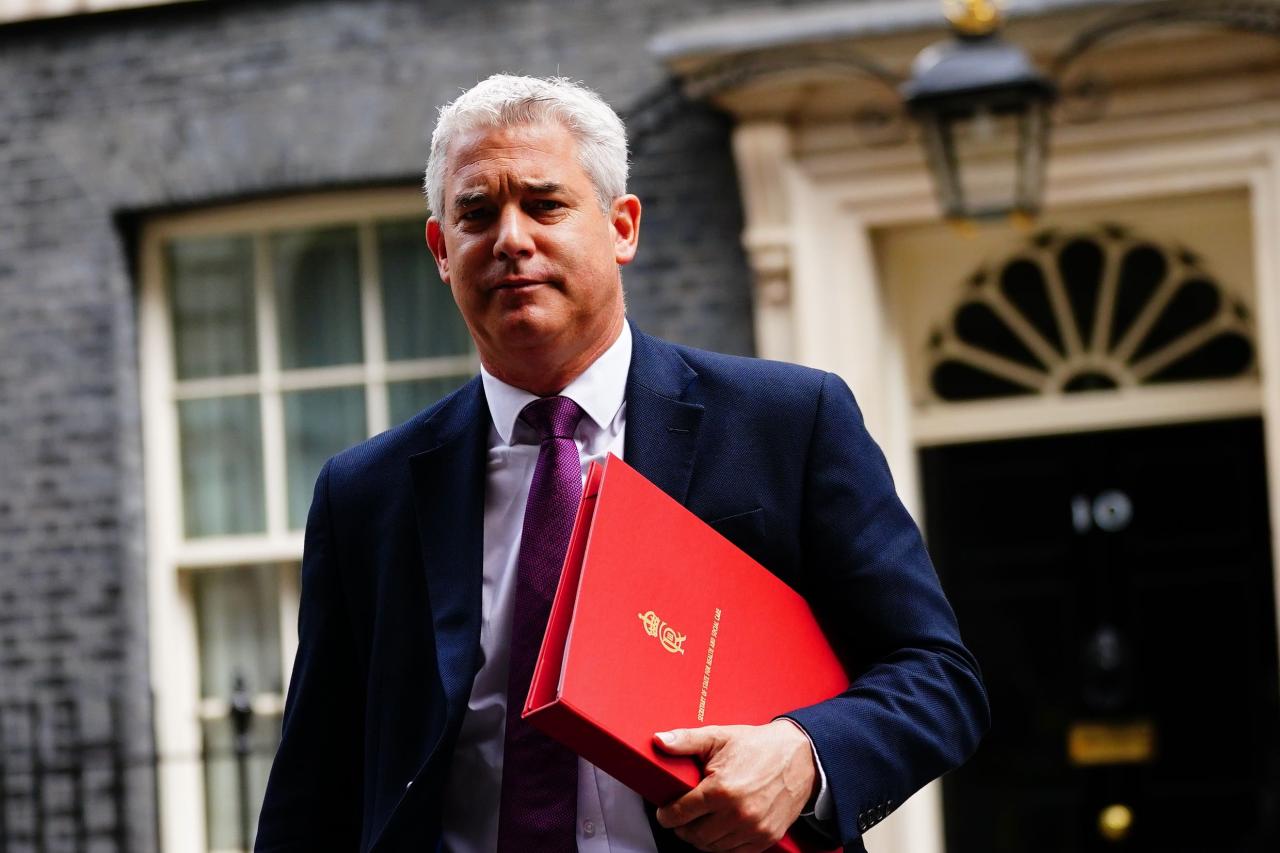
The UK Health Secretary’s Response
The UK Health Secretary would likely be deeply concerned by the doctor’s statement, especially given the potential ramifications for the government’s vaccination strategy. The statement could create a ripple effect, raising anxieties among the public and potentially leading to increased hesitancy towards vaccination.
The Health Secretary’s response would likely involve a combination of damage control and reiterating the importance of vaccination.
Potential Political Ramifications
The doctor’s statement could significantly impact the government’s vaccination strategy, potentially causing a drop in vaccination rates and undermining public trust in the government’s handling of the pandemic. The statement could also be exploited by opposition parties, further fueling political tensions and potentially impacting the government’s standing in the upcoming elections.
Impact on the Government’s Vaccination Strategy, I do not want to have a vaccination nhs doctor tells uk health secretary
The doctor’s statement could lead to a decline in public confidence in the vaccination program, potentially leading to a drop in vaccination rates. This could hinder the government’s efforts to achieve herd immunity and could result in prolonged lockdowns and restrictions.
The statement could also force the government to reconsider its communication strategy and invest more resources in addressing public concerns and misinformation surrounding the vaccination program.
Concluding Remarks: I Do Not Want To Have A Vaccination Nhs Doctor Tells Uk Health Secretary
This statement serves as a stark reminder of the ongoing challenges in navigating the complex landscape of vaccination. It underscores the importance of open dialogue, informed consent, and addressing public concerns with empathy and transparency. Ultimately, the goal should be to foster a society where vaccination is viewed as a tool for safeguarding health, not a source of division or mistrust.