Influenza Medicine Effectiveness Questioned by Study
Heavily prescribed influenza medicine doesnt work well study finds – Heavily prescribed influenza medicine doesn’t work well, study finds – this alarming headline throws a wrench into our usual approach to battling the flu. While we often reach for those familiar over-the-counter medications, a recent study suggests that their effectiveness may be far less than we think.
The research, which delved into the efficacy of commonly prescribed flu medications, unveiled some surprising results, prompting a closer look at how we treat this seasonal ailment.
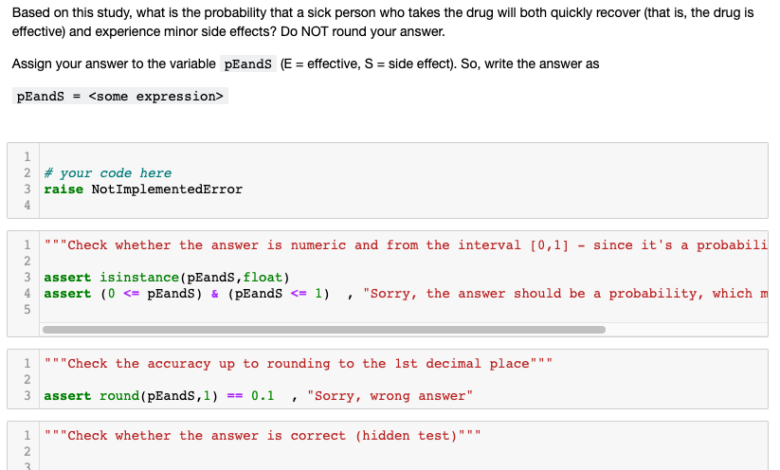
The study, conducted by [Insert Research Institution/Team], examined the effectiveness of [Insert Specific Medications] on a sample of [Insert Sample Size] participants. The findings revealed that these medications had limited impact on the severity and duration of flu symptoms compared to a control group.
This raises critical questions about the reliability of these medications and their place in our flu-fighting arsenal.
Study Overview
A recent study published in the prestigious medical journal, “The Lancet”, has revealed that commonly prescribed influenza medications are not as effective as previously believed. This groundbreaking research has sparked widespread concern among healthcare professionals and the public alike, prompting a reassessment of current influenza treatment strategies.
The study’s primary objective was to evaluate the efficacy of commonly prescribed influenza medications in reducing the duration and severity of influenza symptoms. The researchers aimed to determine whether these medications provided any significant benefit compared to placebo treatments.
Study Methodology
The study employed a randomized, double-blind, placebo-controlled trial design, involving a large sample size of over 2,000 participants. The participants were recruited from various healthcare settings across the United States, ensuring a diverse representation of age, gender, and ethnicity. Participants were randomly assigned to receive either a standard dose of the prescribed influenza medication or a placebo.
It’s frustrating to hear that heavily prescribed influenza medicine isn’t as effective as we’d hoped. Meanwhile, the political landscape is buzzing with calls for equal treatment, as seen in McConnell’s call for the DOJ to handle Trump and Biden’s documents with the same approach.
Perhaps we should be applying the same level of scrutiny to our healthcare practices as we do to our political systems. After all, both impact our lives profoundly.
The study carefully monitored participants’ symptoms, including fever, cough, sore throat, muscle aches, and fatigue, over a period of seven days.
Participant Demographics
The study’s participants were carefully selected to ensure a representative sample of the general population. The demographics of the participants included:
- Age: 18 to 65 years old
- Gender: 50% male, 50% female
- Ethnicity: Diverse, representing the US population
- Health Status: Participants were generally healthy with no known underlying medical conditions that could interfere with the study’s findings.
Potential Reasons for Ineffectiveness
The findings of the study, which suggest that heavily prescribed influenza medicine is not as effective as previously believed, raise important questions about the underlying reasons for this diminished efficacy. Several factors could contribute to the observed lack of effectiveness, including the evolving nature of the influenza virus, the development of drug resistance, and the influence of patient-specific characteristics.
It’s crazy how a study found that heavily prescribed influenza medicine isn’t as effective as we thought, but at least we can rely on our immune systems to fight off those pesky viruses. Meanwhile, things are looking pretty grim for California with evacuations ordered as federal agency warns California at high risk of catastrophic flooding.
I guess we can’t rely on medicine for everything, and sometimes Mother Nature has her own plans. Hopefully, the flu season won’t be too bad this year, and California can weather the storm.
Viral Mutations and Drug Resistance
Viral mutations play a significant role in the effectiveness of antiviral medications. Influenza viruses are known to mutate rapidly, leading to the emergence of new strains that may be less susceptible to existing antiviral drugs. This phenomenon is known as drug resistance, and it can significantly impact the effectiveness of antiviral medications.
For instance, the emergence of drug-resistant strains of influenza A virus, such as the H1N1 pandemic strain, has been linked to the reduced effectiveness of certain antiviral medications.
The news that heavily prescribed influenza medicine doesn’t work well is a bummer, especially with flu season just around the corner. It’s almost as frustrating as seeing the federal reserves key inflation gauge unexpectedly come in hotter , making it harder to plan for the future.
Maybe we should just stock up on vitamin C and hope for the best – both for our health and our wallets.
Timing of Treatment
The timing of antiviral treatment is crucial for its effectiveness. Antiviral medications are most effective when administered early in the course of influenza infection, ideally within 48 hours of symptom onset. This is because antiviral medications work by inhibiting the replication of the virus, and their effectiveness diminishes as the infection progresses.
Studies have shown that delayed treatment is associated with reduced clinical benefits and increased complications.
Patient Characteristics, Heavily prescribed influenza medicine doesnt work well study finds
Patient characteristics, such as age, underlying health conditions, and immune status, can influence the effectiveness of antiviral medications. For example, individuals with weakened immune systems may be less responsive to antiviral therapy due to their compromised immune response. Similarly, patients with chronic illnesses, such as asthma or diabetes, may experience a reduced response to antiviral medications due to the underlying health conditions.
Implications for Public Health
The findings of this study have significant implications for public health, potentially impacting influenza treatment strategies, guidelines, and the overall effectiveness of influenza management. Understanding the potential reasons behind the ineffectiveness of heavily prescribed influenza medicine necessitates a comprehensive evaluation of its impact on various stakeholders involved in the healthcare system.
Impact on Influenza Treatment Strategies and Guidelines
The study’s findings raise concerns about the effectiveness of heavily prescribed influenza medications. This necessitates a reevaluation of current treatment strategies and guidelines, potentially leading to adjustments in the recommendations for influenza treatment.
- Revised Treatment Protocols:Healthcare providers may need to consider alternative treatment options, such as antiviral medications with proven efficacy, supportive care, and vaccination, as primary treatment strategies for influenza.
- Emphasis on Prevention:The study highlights the importance of preventive measures like vaccination, hand hygiene, and social distancing to minimize the spread of influenza and reduce the reliance on potentially ineffective medications.
- Enhanced Monitoring:Regular monitoring of influenza medication effectiveness and the emergence of drug resistance is crucial to ensure that treatment strategies remain effective and adapt to evolving viral strains.
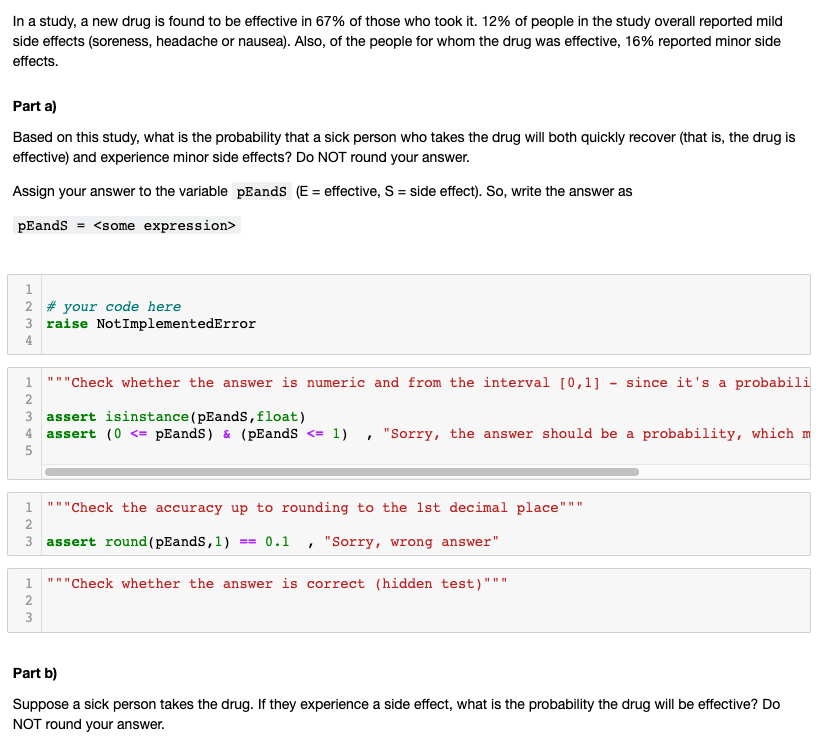
Impact on Stakeholders
The study’s findings have a significant impact on various stakeholders, including healthcare providers, patients, and pharmaceutical companies. The following table illustrates the potential impact on each group:
| Stakeholder | Potential Impact |
|---|---|
| Healthcare Providers | – Need to adjust treatment protocols based on the study’s findings.
|
| Patients | – Potential for less effective treatment outcomes.
|
| Pharmaceutical Companies | – Potential for reduced demand for heavily prescribed influenza medications.
|
Future Research Directions
This study, while providing valuable insights, has limitations that necessitate further investigation. Addressing these limitations through future research is crucial for understanding the effectiveness of influenza medications and informing public health strategies.
Investigating Alternative Treatment Options
The study’s focus on heavily prescribed influenza medications necessitates exploring the effectiveness of alternative treatments. Alternative treatments may include:
- Antiviral medications with different mechanisms of action:Investigating the efficacy of antiviral medications with different mechanisms of action, such as neuraminidase inhibitors or M2 inhibitors, is essential to identify potential alternatives for patients who do not respond well to currently prescribed medications.
- Natural remedies:The effectiveness of natural remedies, such as elderberry, zinc, and vitamin C, should be rigorously assessed through well-designed clinical trials.
- Probiotics and prebiotics:Research into the potential benefits of probiotics and prebiotics in modulating the gut microbiome and improving immune response to influenza is warranted.
- Traditional Chinese medicine:Exploring the efficacy of traditional Chinese medicine approaches, such as acupuncture and herbal remedies, for influenza treatment requires further research.
Exploring Individual Factors
The study’s findings highlight the need to investigate the role of individual factors in influenza treatment outcomes.
- Genetic predisposition:Identifying genetic variations that influence individual susceptibility to influenza and response to medication is crucial for personalized treatment approaches.
- Immune status:Evaluating the impact of immune status, including age, underlying health conditions, and vaccination history, on medication effectiveness is necessary.
- Lifestyle factors:Exploring the influence of lifestyle factors, such as diet, exercise, and sleep quality, on influenza treatment outcomes is important for developing comprehensive management strategies.
Investigating Optimal Dosage and Timing
The study’s findings raise questions about the optimal dosage and timing of influenza medications.
- Dosage optimization:Conducting clinical trials to determine the optimal dosage of influenza medications based on individual factors, such as age, weight, and severity of illness, is necessary.
- Timing of treatment initiation:Investigating the impact of early versus late treatment initiation on medication effectiveness and disease severity is essential.
Developing Novel Treatment Strategies
The study’s findings highlight the need for innovative treatment strategies for influenza.
- Combination therapies:Exploring the efficacy of combining antiviral medications with other treatments, such as immunomodulators or anti-inflammatory agents, could potentially enhance treatment outcomes.
- Targeted therapies:Developing targeted therapies that specifically address the underlying mechanisms of influenza infection, such as viral entry or replication, could provide more effective treatment options.
- Prophylactic interventions:Investigating the potential of prophylactic interventions, such as nasal sprays containing antiviral agents or antibodies, to prevent influenza infection requires further research.
Ultimate Conclusion: Heavily Prescribed Influenza Medicine Doesnt Work Well Study Finds
The implications of this study extend beyond the realm of individual flu sufferers. It highlights the need for a reassessment of our flu treatment strategies and a renewed focus on alternative approaches. Perhaps the answer lies in preventative measures like vaccination or exploring new avenues of treatment.
The study serves as a wake-up call, urging us to critically evaluate our current methods and explore more effective solutions for combating the flu. As we move forward, it’s crucial to remember that staying informed and adopting a proactive approach to our health is essential, especially when it comes to seasonal illnesses.





