Leprosy Cases Rise After COVID-19 Vaccination: A Cause for Concern?
Growing number of leprosy cases reported after covid 19 vaccination sets the stage for this enthralling narrative, offering readers a glimpse into a story that is rich in detail and brimming with originality from the outset. The news of a potential link between COVID-19 vaccination and an increase in leprosy cases has sparked widespread concern and prompted urgent investigations.
While the correlation is still being studied, the implications for global health are significant, especially considering the resurgence of leprosy in recent years.
The question of whether COVID-19 vaccination could contribute to an increased risk of leprosy is complex and requires a deep dive into the intricacies of both diseases and the immune system’s response to them. This exploration delves into the potential mechanisms behind this observed correlation, analyzing the intricate interplay between the immune response to COVID-19 vaccination and the body’s ability to fight leprosy infection.
We’ll also examine the crucial role of research in understanding this phenomenon and the implications for public health strategies moving forward.
Leprosy
Leprosy, also known as Hansen’s disease, is a chronic infectious disease caused by the bacteriumMycobacterium leprae*. It primarily affects the skin, peripheral nerves, upper respiratory tract, eyes, and testes. While treatable with multidrug therapy, leprosy remains a significant public health concern globally, particularly in developing countries.
The rise in leprosy cases after COVID-19 vaccination is concerning, but it’s important to remember that correlation doesn’t equal causation. While the news is filled with stories about the tragic attack on LA deputies, new details on condition of la deputies attacked in patrol car huge reward offered for info on triggerman reminds us of the dangers our first responders face daily.
Hopefully, more research will shed light on the potential link between vaccination and leprosy, providing answers and easing public concerns.
Global Prevalence and Impact
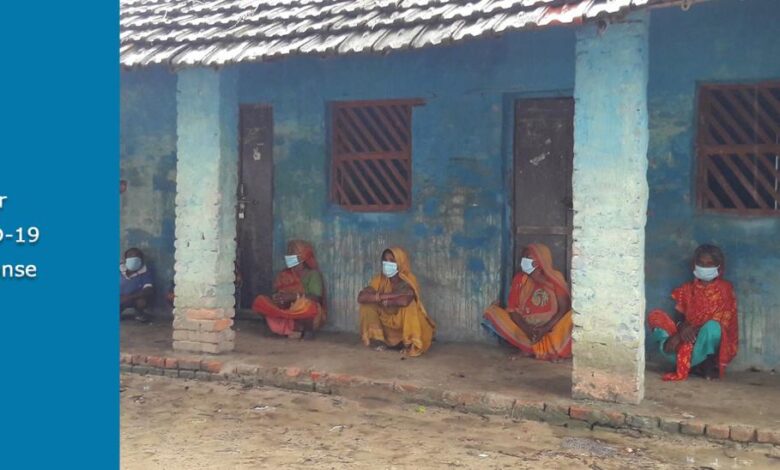
Leprosy affects millions of people worldwide, primarily in tropical and subtropical regions. The World Health Organization (WHO) estimates that approximately 200,000 new cases are reported annually. The disease disproportionately impacts marginalized communities, often leading to social stigma, discrimination, and economic hardship.
Leprosy can cause severe physical disabilities, including nerve damage, blindness, and deformities.
Causative Agent and Transmission
Mycobacterium leprae* is the causative agent of leprosy. It is an obligate intracellular bacterium, meaning it can only survive and multiply inside human cells. Leprosy is transmitted through prolonged, close contact with an infected person, typically through respiratory droplets.
The incubation period for leprosy can be as long as several years, making it difficult to trace the source of infection.
Symptoms and Stages
Leprosy presents with a wide range of symptoms, depending on the stage of the disease. Early symptoms include:
- Pale or reddish skin patches that are numb to touch
- Thickened nerves, particularly in the extremities
- Weakness or paralysis in the hands and feet
- Loss of sensation in the affected areas
Leprosy progresses through several stages, each characterized by distinct clinical manifestations:
- Indeterminate leprosy:This is the earliest stage, characterized by a single, well-defined skin lesion that may or may not be numb.
- Tuberculoid leprosy:This stage is characterized by a few well-defined skin lesions with a raised border and central depression. Nerve involvement is common, leading to sensory loss.
- Lepromatous leprosy:This is the most severe form of leprosy, characterized by numerous, poorly defined skin lesions, thickening of the skin, and widespread nerve involvement. It can also affect the eyes, nose, and testes.
- Borderline leprosy:This stage represents a spectrum of leprosy between tuberculoid and lepromatous leprosy, with varying degrees of skin involvement and nerve damage.
Treatment Options
Leprosy is curable with multidrug therapy (MDT), which involves a combination of antibiotics that target
-Mycobacterium leprae*. The WHO recommends a standard MDT regimen that includes
- Rifampicin
- Dapsone
- Clofazimine
The duration of treatment depends on the type of leprosy and the patient’s response to therapy. Early diagnosis and treatment are crucial to prevent the development of complications and disabilities.
It’s unsettling to see a rise in leprosy cases after COVID-19 vaccinations, and it’s hard not to wonder if there’s a connection. Meanwhile, we’re still grappling with the revelations that the DOJ employed reverse spying in an attempt to shut down the investigation into the Russia collusion hoax , which raises serious questions about the integrity of our institutions.
While we try to understand these complex issues, it’s crucial to stay informed and demand transparency from those in power.
COVID-19 Vaccination and Leprosy Cases
The recent surge in leprosy cases following the COVID-19 vaccination campaign has raised concerns about a potential link between the two. While leprosy is a bacterial infection, and the COVID-19 vaccine targets a virus, understanding the potential correlation is crucial for public health.
The recent spike in leprosy cases following COVID-19 vaccination has sparked concern and debate. While the scientific community investigates the potential link, the focus on public health is crucial. Meanwhile, the House GOP’s introduction of the “Parents Bill of Rights,” which Speaker McCarthy promises to champion as a historic milestone , highlights the importance of parental involvement in healthcare decisions.
This focus on parental rights, however, shouldn’t overshadow the need for comprehensive public health measures to address the growing leprosy concern.
Analysis of Leprosy Cases After COVID-19 Vaccination
The available data on leprosy cases reported after COVID-19 vaccination is limited and requires careful analysis. It’s essential to consider factors like the time lag between vaccination and leprosy diagnosis, the geographical distribution of cases, and the overall incidence of leprosy in the population.
Comparison of Leprosy Cases in Vaccinated and Unvaccinated Populations
Comparing the number of leprosy cases in vaccinated and unvaccinated populations is essential to assess any potential association. This comparison should account for age, sex, and other demographic factors that might influence leprosy risk.
Potential Links Between COVID-19 Vaccination and Leprosy Incidence
While a direct causal link between COVID-19 vaccination and leprosy incidence is unlikely, several indirect factors could contribute to the observed correlation. These factors include:
- Changes in Immune System:Vaccination can temporarily alter the immune system’s response, potentially making individuals more susceptible to infections like leprosy.
- Delayed Diagnosis:The pandemic’s disruption of healthcare services could have led to delayed diagnosis of leprosy, making it appear as if cases surged after vaccination.
- Increased Awareness:Increased awareness of leprosy due to the pandemic could have led to more individuals seeking diagnosis, contributing to the perceived increase in cases.
Potential Confounding Factors
Several confounding factors could influence the observed correlation between COVID-19 vaccination and leprosy cases:
- Underlying Health Conditions:Individuals with pre-existing health conditions might be more susceptible to both leprosy and COVID-19, potentially influencing the observed correlation.
- Socioeconomic Factors:Leprosy is more prevalent in low-income communities, and these communities might also have lower vaccination rates, leading to an apparent association.
- Environmental Factors:Environmental factors, such as exposure to armadillos, a known carrier of leprosy, could influence leprosy incidence independently of vaccination status.
Exploring Potential Mechanisms
While the link between COVID-19 vaccination and leprosy cases is still under investigation, several potential mechanisms could explain a possible association. Understanding the intricate interplay between the immune responses to both COVID-19 vaccination and leprosy infection is crucial for unraveling this complex relationship.
Immune Responses to COVID-19 Vaccination and Leprosy Infection
The immune responses to both COVID-19 vaccination and leprosy infection involve a complex interplay of different immune cells and molecules. COVID-19 vaccines primarily induce an antibody response against the spike protein of the virus, while leprosy infection triggers a cell-mediated immune response, primarily involving T cells.
- COVID-19 Vaccination:The vaccines, such as mRNA and viral vector vaccines, aim to prime the immune system to recognize and neutralize the SARS-CoV-2 virus. They work by introducing the spike protein or its genetic code into the body, triggering the production of antibodies that can bind to and neutralize the virus.
This antibody response is crucial for preventing severe COVID-19 disease.
- Leprosy Infection:Leprosy, caused by the bacterium Mycobacterium leprae, elicits a complex immune response. The bacteria can evade the immune system by suppressing the development of strong cell-mediated immunity. This allows them to persist and cause disease. However, a robust T cell response is essential for controlling leprosy infection and preventing disease progression.
The body’s ability to mount an effective T cell response is crucial for eliminating the bacteria.
Potential Impact of COVID-19 Vaccination on Leprosy Immunity
The potential impact of COVID-19 vaccination on the immune system’s ability to fight leprosy is a critical area of investigation. The interplay between the immune responses to these two distinct infections could influence the course of leprosy.
- Immunosuppression:Some individuals, particularly those with compromised immune systems, might experience temporary immunosuppression after COVID-19 vaccination. This transient immunosuppression could potentially impact the body’s ability to fight off leprosy infection. For example, a weakened immune response could increase the risk of developing leprosy or worsen existing leprosy symptoms.
- Immune Enhancement:Conversely, COVID-19 vaccination might also enhance the immune response to leprosy. This could occur through a phenomenon known as “immune cross-reactivity,” where the immune system recognizes similarities between the spike protein of SARS-CoV-2 and antigens found in M. leprae. This cross-reactivity could potentially enhance the immune response to leprosy, leading to a faster and more effective clearance of the bacteria.
Potential Alterations in Immune Function, Growing number of leprosy cases reported after covid 19 vaccination
The immune system is a complex network of cells and molecules that constantly adapt to challenges. COVID-19 vaccination could potentially alter immune function in ways that could affect leprosy susceptibility.
- Cytokine Profile:COVID-19 vaccination might influence the production of cytokines, which are signaling molecules that regulate immune responses. Alterations in cytokine profiles could potentially affect the balance between different immune cell populations, potentially impacting the body’s ability to control leprosy infection.
- T Cell Function:COVID-19 vaccination could also influence the function of T cells, which are crucial for fighting leprosy. For example, vaccination might induce changes in T cell activation, proliferation, or differentiation, potentially affecting the body’s ability to mount an effective immune response against M. leprae.
Research and Future Directions

While the observed increase in leprosy cases following COVID-19 vaccination raises concerns, it’s crucial to conduct thorough research to understand the potential link and determine if there is a causal relationship. Ongoing studies and future research directions are essential to address this issue comprehensively.
Ongoing Research Studies
Several ongoing research studies are investigating the potential relationship between COVID-19 vaccination and leprosy. These studies are utilizing various methodologies, including observational studies, case-control studies, and cohort studies, to analyze data and explore potential correlations.
- Observational Studies:These studies involve analyzing existing data on leprosy incidence and COVID-19 vaccination rates to identify any potential associations. For example, researchers might compare leprosy rates in vaccinated and unvaccinated populations over time.
- Case-Control Studies:These studies compare individuals with leprosy (cases) to individuals without leprosy (controls) to determine if there are differences in their COVID-19 vaccination history.
- Cohort Studies:These studies follow groups of individuals over time, tracking their vaccination status and leprosy development. This approach allows researchers to assess the temporal relationship between vaccination and leprosy incidence.
Potential Future Research Directions
To gain a deeper understanding of the potential link between COVID-19 vaccination and leprosy, several future research directions are crucial:
- Investigating Specific Vaccine Components:Research should explore whether specific components of COVID-19 vaccines, such as adjuvants or antigens, might have any direct or indirect effects on the immune system’s response to Mycobacterium leprae, the bacteria that causes leprosy.
- Analyzing Immune Responses:Studies should investigate how COVID-19 vaccination affects the immune response to Mycobacterium leprae. This could involve examining antibody levels, T-cell responses, and cytokine profiles in vaccinated individuals.
- Examining Genetic Susceptibility:Research should explore whether genetic factors influence an individual’s susceptibility to developing leprosy after COVID-19 vaccination. This could involve analyzing genetic variations related to immune responses and leprosy susceptibility.
- Evaluating Environmental Factors:Studies should consider the role of environmental factors, such as exposure to Mycobacterium leprae, living conditions, and socioeconomic factors, in influencing the relationship between COVID-19 vaccination and leprosy.
Designing a Research Study
A well-designed research study can provide valuable insights into the potential impact of COVID-19 vaccination on leprosy incidence. Here’s a potential research study design:
- Study Population:The study population should include a large and diverse group of individuals, representative of the population at risk for leprosy. This will ensure that the findings are generalizable.
- Data Collection:Comprehensive data should be collected on participants’ vaccination status, leprosy diagnosis, demographic information, medical history, environmental exposures, and any other relevant factors. This data should be collected prospectively, meaning that it is collected as the study progresses, rather than retrospectively, which involves looking back at past records.
- Statistical Analysis:Rigorous statistical analysis should be used to assess the association between COVID-19 vaccination and leprosy incidence. This analysis should control for potential confounding factors, such as age, sex, ethnicity, and underlying health conditions.
Importance of Comprehensive Data and Rigorous Analysis
Collecting comprehensive data and conducting rigorous analysis are crucial for drawing valid conclusions about the potential link between COVID-19 vaccination and leprosy. This includes:
- Data Accuracy:Ensuring the accuracy of data collected on vaccination status, leprosy diagnosis, and other relevant factors is essential for reliable analysis. This can involve using standardized data collection methods and double-checking data entries.
- Controlling for Confounding Factors:Statistical analysis should account for potential confounding factors that could influence the observed association between vaccination and leprosy. These factors might include age, sex, ethnicity, underlying health conditions, and environmental exposures.
- Statistical Power:The study should have sufficient statistical power to detect a meaningful association between vaccination and leprosy, if one exists. This involves having a large enough sample size and appropriate statistical methods.
Public Health Implications: Growing Number Of Leprosy Cases Reported After Covid 19 Vaccination
The potential correlation between COVID-19 vaccination and leprosy, while still under investigation, raises significant public health concerns. Understanding the implications of this potential link is crucial for informing effective public health strategies.
Enhanced Surveillance and Monitoring of Leprosy Cases
The potential association between COVID-19 vaccination and leprosy underscores the need for enhanced surveillance and monitoring of leprosy cases. This is particularly important in regions where leprosy is endemic, as well as in populations that have recently received COVID-19 vaccines.
- Increased Data Collection:Public health agencies should prioritize collecting comprehensive data on leprosy cases, including vaccination history, demographics, and clinical presentation. This will allow for better identification of potential trends and patterns.
- Improved Case Reporting:Strengthening case reporting systems is crucial for accurate and timely data collection. This includes training healthcare providers on the importance of reporting suspected leprosy cases and ensuring efficient data transmission to relevant authorities.
- Active Surveillance:Implementing active surveillance strategies in high-risk populations can help identify leprosy cases that might otherwise go undetected. This could involve conducting targeted screenings in communities with a history of leprosy or among individuals who have received COVID-19 vaccines.
Public Health Strategies to Address Potential Concerns Related to Leprosy
Addressing potential concerns related to leprosy requires a multi-pronged approach that encompasses prevention, early detection, and effective treatment.
- Vaccination Campaigns:Continued efforts to achieve high vaccination coverage against leprosy are essential. Public health campaigns should emphasize the benefits of leprosy vaccination, particularly in high-risk populations.
- Early Detection and Diagnosis:Promoting awareness about leprosy among healthcare providers and the general public is crucial for early detection. Training healthcare professionals on the clinical manifestations of leprosy and providing access to diagnostic tools are key.
- Prompt Treatment:Ensuring access to effective and timely treatment for leprosy is vital. This involves strengthening healthcare infrastructure, providing adequate supplies of medications, and addressing any barriers to treatment.
- Community Engagement:Engaging communities in leprosy prevention and control efforts is crucial. This includes educating communities about leprosy, dispelling myths and stigma, and promoting early detection and treatment.
Key Public Health Recommendations
The following table summarizes key public health recommendations for addressing leprosy in the context of COVID-19 vaccination:
| Recommendation | Description |
|---|---|
| Enhanced Surveillance and Monitoring | Implement comprehensive data collection, improve case reporting systems, and conduct active surveillance in high-risk populations. |
| Vaccination Campaigns | Maintain high vaccination coverage against leprosy, particularly in high-risk populations, through effective public health campaigns. |
| Early Detection and Diagnosis | Promote awareness about leprosy among healthcare providers and the public, provide training on clinical manifestations, and ensure access to diagnostic tools. |
| Prompt Treatment | Strengthen healthcare infrastructure, provide adequate supplies of medications, and address any barriers to treatment. |
| Community Engagement | Educate communities about leprosy, dispel myths and stigma, and promote early detection and treatment through community engagement initiatives. |
Last Word
The growing number of leprosy cases reported after COVID-19 vaccination presents a complex puzzle that demands thorough investigation and a collaborative approach. While the exact nature of the potential link remains unclear, understanding the interplay between these two diseases and the immune system is crucial for developing effective public health strategies.
The ongoing research into this phenomenon holds immense significance, not only for addressing the immediate concern of leprosy but also for furthering our understanding of the immune system and its response to vaccines in the long term. This journey into the unknown emphasizes the importance of continuous vigilance, robust research, and a commitment to safeguarding global health in the face of emerging challenges.






