COVID-19 Vaccines Did the CDC Change the Definition?
Covid 19 vaccines didnt work so cdc changed the definition of vaccines – COVID-19 vaccines didn’t work so CDC changed the definition of vaccines – a statement that has been circulating online, sparking debate and raising concerns about the effectiveness of vaccines. This claim, while seemingly shocking, requires careful examination. It’s crucial to understand the evolution of vaccine definitions, the scientific evidence supporting the effectiveness of COVID-19 vaccines, and the role of the CDC in public health.
The statement that the CDC changed the definition of vaccines is a misrepresentation of the facts. While the CDC has clarified its definition of “vaccine” over time, this change was not driven by the ineffectiveness of COVID-19 vaccines. It was a natural evolution in response to the scientific understanding of vaccines and the need for clear communication with the public.
The Evolution of Vaccine Definitions
The definition of a “vaccine” has evolved over time, reflecting advancements in scientific understanding and the development of new technologies. This evolution is particularly evident in the context of the COVID-19 pandemic, where the emergence of novel vaccine technologies like mRNA vaccines prompted a reassessment of traditional definitions.
The Historical Context of Vaccine Definitions
The concept of vaccination dates back to the 18th century, when Edward Jenner first demonstrated the efficacy of cowpox inoculation in protecting against smallpox. Early vaccines, like the smallpox vaccine, relied on weakened or inactivated forms of the target pathogen. These early vaccines primarily aimed to induce an immune response against the pathogen’s specific antigens.
A Timeline of CDC Vaccine Definitions
The Centers for Disease Control and Prevention (CDC) has played a crucial role in defining and promoting vaccination in the United States. The CDC’s definition of “vaccine” has undergone several revisions over the years, reflecting changes in scientific understanding and the emergence of new vaccine technologies.
- Early Definitions: The CDC’s initial definition of “vaccine” focused on the use of weakened or inactivated pathogens. These definitions were based on the understanding of vaccines as traditional biological preparations.
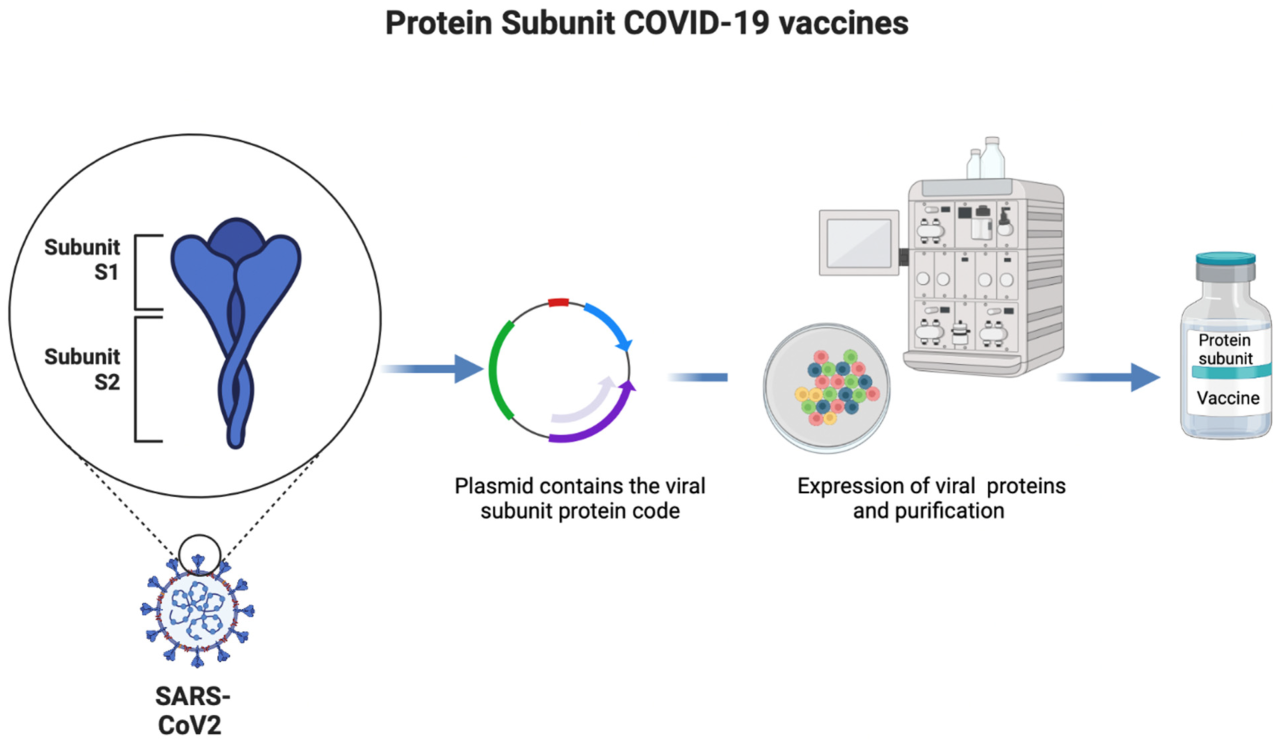
- Expanding Definitions: As vaccine technologies advanced, the CDC’s definition evolved to encompass a broader range of approaches, including the use of toxoids, subunit vaccines, and recombinant vaccines. These revisions reflected the growing understanding of the immune system and the diverse ways in which vaccines could stimulate an immune response.
- The COVID-19 Era: The emergence of mRNA vaccines during the COVID-19 pandemic led to a further evolution in the CDC’s definition of “vaccine.” This definition now encompasses vaccines that utilize genetic material, such as mRNA, to induce an immune response.
The CDC’s Definition of “Vaccine” Before and After the COVID-19 Pandemic
The CDC’s definition of “vaccine” before the COVID-19 pandemic primarily focused on traditional vaccine technologies, such as those utilizing weakened or inactivated pathogens. This definition was based on the understanding of vaccines as biological preparations that directly introduce a pathogen or its components into the body.After the emergence of mRNA vaccines, the CDC expanded its definition to include vaccines that utilize genetic material to induce an immune response.
This expanded definition acknowledges the emergence of new vaccine technologies and reflects the evolving understanding of how vaccines can stimulate immunity.
It’s been a wild ride with the COVID-19 vaccines, and the CDC’s changing definition of “vaccine” speaks volumes. It seems like they’re scrambling to maintain the narrative, even though the results haven’t been what they promised. At least we have some good news with Fauci’s resignation being good news for America, according to Rep. Buddy Carter. Perhaps now we can move towards a more transparent and honest approach to public health, where the focus is on real solutions, not just controlling the narrative.
After all, if the vaccines aren’t working as advertised, why are we still clinging to a definition that doesn’t reflect reality?
“A vaccine is a preparation that is used to stimulate the body’s immune system to protect against a specific disease.” – CDC
The COVID-19 Vaccine and its Effectiveness
The COVID-19 vaccines have been instrumental in reducing the severity of the pandemic, saving countless lives and easing the strain on healthcare systems worldwide. These vaccines have been rigorously tested and proven effective in preventing severe illness, hospitalization, and death from COVID-19.
Scientific Evidence Supporting Vaccine Effectiveness
A vast body of scientific evidence supports the effectiveness of COVID-19 vaccines. Numerous studies have demonstrated their ability to significantly reduce the risk of severe illness, hospitalization, and death. For instance, a large-scale study published in the New England Journal of Medicine found that the Pfizer-BioNTech vaccine was 95% effective in preventing symptomatic COVID-19 in individuals who received two doses.
Similar results have been observed for other vaccines, such as Moderna and Johnson & Johnson.
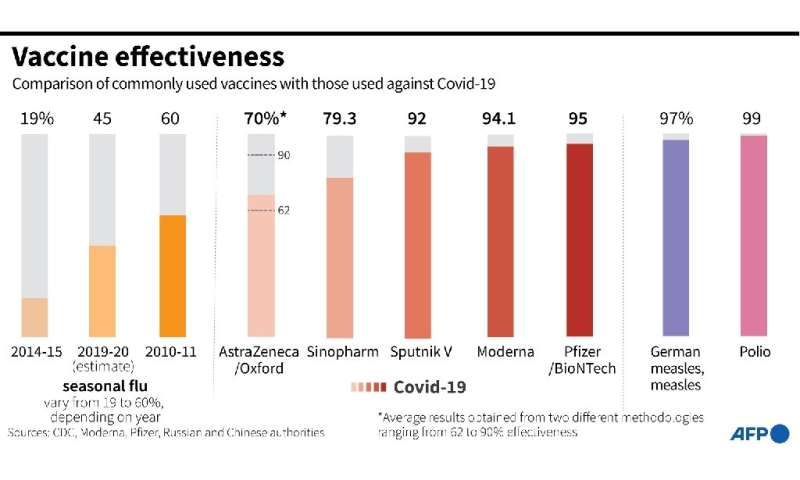
Types of COVID-19 Vaccines and Their Efficacy Rates
There are several types of COVID-19 vaccines available, each with its unique mechanism of action and efficacy rate.
The whole “COVID-19 vaccines didn’t work” narrative is a bit of a red herring, especially when you consider the CDC’s shifting definition of “vaccine.” It’s more about the changing landscape of the virus itself and the evolving understanding of immunity. Meanwhile, the recent jobs report shows hiring slowdown inflation pressures elevated , which could be a sign of a cooling economy.
This might be a good time to revisit the whole “vaccines didn’t work” argument and see if it holds up against the backdrop of a potentially changing economic climate.
- mRNA Vaccines (Pfizer-BioNTech and Moderna): These vaccines use messenger RNA (mRNA) to instruct the body to produce a harmless piece of the spike protein found on the surface of the SARS-CoV-2 virus. This triggers an immune response, preparing the body to fight off infection if exposed to the real virus. The efficacy rates for these vaccines have been consistently high, with studies showing a reduction of 90% or more in the risk of symptomatic COVID-19.
- Viral Vector Vaccines (Johnson & Johnson and AstraZeneca): These vaccines use a harmless, modified virus (a viral vector) to deliver genetic material that codes for the spike protein. This genetic material instructs the body to produce the spike protein, triggering an immune response. While slightly less effective than mRNA vaccines, viral vector vaccines still offer significant protection against severe illness, hospitalization, and death.
- Protein Subunit Vaccines (Novavax): These vaccines use a specific part of the virus (the spike protein) to stimulate an immune response. This approach has been used in other vaccines, such as the influenza vaccine, and is generally considered safe and effective. The Novavax vaccine has shown an efficacy rate of over 90% in clinical trials.
Vaccine Breakthrough Infections and Their Impact on Disease Transmission
While vaccines are highly effective in preventing severe illness, hospitalization, and death, they do not always prevent infection entirely. A vaccine breakthrough infection occurs when a fully vaccinated person gets infected with COVID-19. These infections are generally milder than in unvaccinated individuals and are less likely to lead to serious complications.
- Factors influencing breakthrough infections: Several factors can contribute to vaccine breakthrough infections, including the emergence of new variants with increased transmissibility, waning immunity over time, and individual factors like age and underlying health conditions.
- Impact on transmission: While breakthrough infections can occur, vaccinated individuals are less likely to transmit the virus to others. Studies have shown that vaccinated individuals are less likely to carry high viral loads, reducing the risk of spreading the virus to others.
The Role of the CDC in Public Health
The Centers for Disease Control and Prevention (CDC) is a leading public health agency in the United States, playing a crucial role in protecting the nation’s health and safety. Its responsibilities encompass a wide range of activities, including disease surveillance, prevention, and control, as well as research and public health communication. The CDC’s role in vaccine recommendations and public health guidance is paramount.
It’s truly alarming to see the CDC redefine “vaccine” after the COVID-19 shots failed to prevent transmission, and then see the Biden administration accused of running the world’s epicenter of child trafficking by a former White House advisor in this article. It makes you wonder if there’s a connection between these two disturbing trends, and if the government is trying to distract us from the failures of the COVID-19 vaccine program.
It establishes guidelines for vaccine use, provides recommendations for immunization schedules, and tracks vaccine safety and effectiveness. These recommendations are based on a rigorous scientific process that involves analyzing data from clinical trials, surveillance systems, and epidemiological studies.
The CDC’s Vaccine Recommendation Process
The CDC’s vaccine recommendations are informed by a comprehensive process that involves multiple steps:
- Review of Scientific Evidence: The CDC’s Advisory Committee on Immunization Practices (ACIP) reviews the latest scientific evidence on the safety, efficacy, and effectiveness of vaccines. This evidence comes from clinical trials, observational studies, and other research sources.
- Expert Consultation: ACIP members, who are experts in infectious diseases, immunology, and public health, discuss the evidence and consider the potential benefits and risks of vaccination.
- Public Comment: The CDC seeks public input on its recommendations through a public comment period, allowing stakeholders to provide feedback and raise concerns.
- Recommendation Development: Based on the evidence, expert consultation, and public input, ACIP develops its recommendations for vaccine use. These recommendations are then presented to the CDC director for final approval.
- Implementation and Monitoring: Once approved, the CDC’s vaccine recommendations are implemented through public health programs and healthcare providers. The CDC also monitors the effectiveness and safety of vaccines through ongoing surveillance and research.
The CDC’s Vaccine Definitions
The CDC defines vaccines as “biological preparations that provide active immunity to a particular disease.” Vaccines work by stimulating the body’s immune system to recognize and fight off specific pathogens. The CDC’s definition of a vaccine has evolved over time to reflect advancements in vaccine technology and understanding of the immune system.
Potential Influence of Political Pressures on CDC Decision-Making
The CDC’s decision-making process has been subject to scrutiny and criticism, with concerns raised about potential political influence on its recommendations. The CDC’s independence and scientific integrity are essential to maintaining public trust in its recommendations. It is crucial for the CDC to prioritize evidence-based decision-making and to resist pressure from political interests that may compromise its scientific objectivity.
Misinformation and Vaccine Hesitancy: Covid 19 Vaccines Didnt Work So Cdc Changed The Definition Of Vaccines
The COVID-19 pandemic has not only been a public health crisis but also a battle against misinformation. The spread of false and misleading information about the virus and its vaccines has fueled vaccine hesitancy, undermining public health efforts. Understanding the nature of this misinformation and its impact is crucial for promoting vaccine confidence and mitigating the pandemic’s effects.
Common Misconceptions About COVID-19 Vaccines
Misinformation about COVID-19 vaccines often stems from a lack of understanding of scientific principles and the complex nature of vaccine development. Here are some common misconceptions:
- Vaccines cause autism: This myth, debunked by numerous scientific studies, originated from a fraudulent paper published in the medical journal The Lancet in 1998. The paper was retracted, and its author lost his medical license.
- Vaccines contain microchips: This conspiracy theory suggests that vaccines are used to track individuals, a claim that lacks any scientific evidence.
- Vaccines alter your DNA: Vaccines do not alter a person’s DNA. They work by introducing a weakened or inactive version of a virus or bacteria, triggering an immune response without causing disease.
- Natural immunity is better than vaccine-induced immunity: While natural infection can provide immunity, it comes with the risk of severe illness, hospitalization, and even death. Vaccines offer a safer and more controlled way to achieve immunity.
The Spread of Misinformation and Its Impact on Public Trust
Misinformation spreads rapidly, particularly through social media and online platforms. This can have a significant impact on public trust in vaccines and lead to vaccine hesitancy.
“The spread of misinformation about COVID-19 vaccines has been a major challenge to public health efforts. It has eroded trust in scientific institutions and contributed to vaccine hesitancy.”Dr. Anthony Fauci, Director of the National Institute of Allergy and Infectious Diseases.
The Role of Social Media and Online Platforms in Disseminating Vaccine-Related Misinformation
Social media platforms, with their vast reach and algorithms that prioritize engagement, have become fertile ground for the spread of misinformation.
- Algorithms that prioritize engagement: Social media algorithms often prioritize content that elicits strong emotions, such as fear or anger, which can contribute to the spread of misinformation.
- Filter bubbles and echo chambers: Social media algorithms can create filter bubbles and echo chambers, where users are only exposed to information that confirms their existing beliefs, making it difficult to challenge misinformation.
- The spread of conspiracy theories: Online platforms can facilitate the formation and spread of conspiracy theories, often presented as credible information, which can undermine trust in scientific institutions.
Public Health Implications
The COVID-19 pandemic has highlighted the crucial role of vaccines in protecting public health. However, vaccine hesitancy and misinformation have posed significant challenges to achieving widespread immunity and controlling the spread of the virus. This section will explore the potential consequences of vaccine hesitancy and misinformation on disease transmission and public health outcomes, analyzing the impact on healthcare systems and resource allocation.
The Impact of Vaccine Hesitancy on Disease Transmission
Vaccine hesitancy refers to the delay in acceptance or refusal of vaccines despite the availability of vaccination services. It can result from various factors, including concerns about vaccine safety, lack of trust in healthcare providers, and misinformation. A significant consequence of vaccine hesitancy is increased disease transmission. When a large proportion of the population remains unvaccinated, the virus can easily spread among susceptible individuals, leading to outbreaks and higher infection rates.
This can overwhelm healthcare systems, leading to strained resources and delays in care.
A study published in the journal Nature found that vaccine hesitancy in the United States contributed to a significant increase in COVID-19 cases and hospitalizations.
The Impact of Vaccine Misinformation on Healthcare Systems, Covid 19 vaccines didnt work so cdc changed the definition of vaccines
Misinformation about vaccines can spread rapidly through social media and other online platforms, often fueled by conspiracy theories and false claims. This can lead to widespread public distrust in vaccines, further exacerbating vaccine hesitancy.
A study by the Pew Research Center found that 77% of Americans believe that the COVID-19 vaccine is safe, but a significant minority (23%) still express concerns about its safety.
The spread of misinformation can also lead to increased demand for healthcare services, as individuals seek unnecessary medical attention or treatment for vaccine-related side effects. This can strain healthcare resources and divert attention from other essential medical needs.
Benefits and Risks of COVID-19 Vaccination
The benefits of COVID-19 vaccination far outweigh the risks. Vaccines have been proven to be highly effective in preventing severe illness, hospitalization, and death from COVID-19. | Benefit | Risk ||—|—|| Reduced risk of severe illness, hospitalization, and death from COVID-19 | Mild side effects such as pain, redness, or swelling at the injection site, fatigue, headache, or muscle aches || Reduced risk of transmission of the virus to others | Rare allergic reactions || Protection against long COVID-19 | Myocarditis (inflammation of the heart muscle), especially in young men || Return to normalcy and reduced economic disruption | Blood clots (rare) || Protection for vulnerable populations | Guillain-Barré syndrome (rare) |It is important to note that the risks associated with COVID-19 vaccination are extremely rare and far outweighed by the benefits.
The COVID-19 pandemic has highlighted the importance of public health communication and the need to combat misinformation. While it’s natural to have questions and concerns about vaccines, it’s essential to rely on credible sources of information, such as the CDC, and to engage in constructive dialogue. By understanding the science behind vaccines and the role of public health organizations, we can make informed decisions about our health and contribute to a healthier society.





