COVID-19 Cases Milder, Upper Respiratory Focus: Doctors Explain
Covid 19 cases become milder with upper respiratory focus doctors say – COVID-19 Cases Milder, Upper Respiratory Focus: Doctors Explain. The pandemic has been a rollercoaster of twists and turns, and one of the latest developments is a shift in the way COVID-19 manifests. Doctors are increasingly observing milder cases with a primary focus on upper respiratory symptoms.
This change has sparked curiosity and questions about the evolution of the virus and its implications for our health and future.
This shift towards milder cases, primarily impacting the upper respiratory system, is a fascinating phenomenon. While it offers a glimmer of hope for a less severe pandemic, it also presents new challenges for understanding the virus’s evolution and adapting our public health strategies.
This blog delves into the reasons behind this change, explores the impact on our immune system, and examines the implications for public health moving forward.
Evolution of COVID-19 Variants
The COVID-19 pandemic has been marked by the emergence of numerous variants of the SARS-CoV-2 virus. These variants have differed in their transmissibility, severity, and even symptoms, posing ongoing challenges to public health efforts. Understanding the evolution of these variants is crucial for developing effective prevention and treatment strategies.
Variants and their Characteristics
The emergence of new variants is a natural consequence of viral evolution. Viruses constantly undergo mutations, some of which can lead to changes in their characteristics. The World Health Organization (WHO) has designated several variants of concern (VOCs) and variants of interest (VOIs) based on their potential impact on public health.
- Alpha (B.1.1.7):First identified in the UK in late 2020, the Alpha variant was highly transmissible and associated with an increased risk of hospitalization. It was characterized by mutations in the spike protein, which helps the virus attach to human cells.
It’s reassuring to hear that COVID-19 cases are becoming milder, primarily affecting the upper respiratory system, according to doctors. However, this news comes amidst a concerning development: thousands of NYC nurses are officially on strike after negotiations with hospitals collapsed.
This strike highlights the ongoing challenges healthcare workers face, particularly in the face of evolving health threats like COVID-19. While the virus may be milder, the pressure on healthcare systems remains, and the nurses’ strike underscores the need for improved working conditions and fair treatment for these vital frontline professionals.
- Beta (B.1.351):This variant, first identified in South Africa in late 2020, also displayed increased transmissibility and was associated with partial immune evasion, meaning it could evade some of the protection provided by vaccines or previous infection.
- Gamma (P.1):First detected in Brazil in early 2021, the Gamma variant was known for its high transmissibility and potential for immune escape. It was also linked to an increased risk of severe disease.
- Delta (B.1.617.2):This variant, first identified in India in late 2020, quickly became the dominant variant globally. It was characterized by its high transmissibility, leading to significant surges in cases and hospitalizations.
- Omicron (B.1.1.529):This variant, first identified in South Africa in late 2021, rapidly became the dominant variant worldwide. Omicron has been associated with a significant increase in transmissibility, but its severity has been debated. While it initially appeared to be less severe, it has been linked to increased hospitalization rates, particularly among unvaccinated individuals.
Mutations and their Impact
The emergence of new variants is driven by mutations in the virus’s genetic material. These mutations can occur randomly or be driven by selective pressures, such as the presence of antibodies from vaccination or previous infection.
- Spike Protein Mutations:Mutations in the spike protein, which is responsible for attaching to human cells, can affect the virus’s transmissibility and its ability to evade the immune system. For example, the D614G mutation, which emerged early in the pandemic, increased the virus’s transmissibility.
It’s interesting to see how COVID-19 is evolving, with doctors now saying cases are becoming milder and focusing more on the upper respiratory system. Meanwhile, the news cycle continues to churn, with recent reports of classified documents found at Penn Biden Center, the president’s lawyer adding to the mix.
It seems like we’re constantly bombarded with new information, both medical and political, making it hard to keep up sometimes. Still, it’s good to know that the severity of COVID-19 appears to be lessening, even as we navigate through these turbulent times.
- Other Mutations:Mutations in other parts of the virus’s genome can also affect its characteristics. For example, mutations in the polymerase gene can affect the virus’s ability to replicate.
Symptom Differences
While early variants of COVID-19 were often associated with fever, cough, shortness of breath, and loss of taste or smell, the symptoms of more recent variants have been observed to be more similar to those of a common cold.
Shift Towards Upper Respiratory Symptoms
The shift towards upper respiratory symptoms, such as runny nose, sore throat, and congestion, may be due to several factors:
- Increased Immunity:As more people have been vaccinated or infected with COVID-19, the virus has faced a more immune population. This may have led to the virus evolving to favor milder symptoms, as it can still spread effectively even if it doesn’t cause severe illness.
- Viral Evolution:The virus may have simply evolved to be more efficient at spreading through the upper respiratory tract, leading to more common cold-like symptoms.
- Variant-Specific Differences:Certain variants may have mutations that make them more likely to cause upper respiratory symptoms than others.
Impact of Vaccination and Immunity
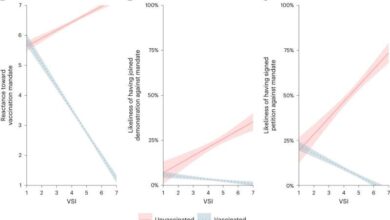
The effectiveness of vaccines and the role of natural immunity are crucial aspects in understanding the ongoing COVID-19 pandemic. While vaccines have significantly reduced severe disease and death, the emergence of new variants has posed challenges. Understanding how vaccination and immunity impact the severity of symptoms and the immune response to evolving variants is vital.
Effectiveness of Vaccines Against Different Variants
Vaccines have been remarkably effective in preventing severe illness, hospitalization, and death from COVID-19. However, the effectiveness of vaccines against different variants can vary.
- Early vaccines were highly effective against the original strain and the Alpha variant.
- With the emergence of the Delta and Omicron variants, vaccine effectiveness against infection decreased, but protection against severe disease remained substantial.
- Booster doses have been shown to enhance protection against infection and severe disease from emerging variants.
The ongoing evolution of COVID-19 necessitates continuous monitoring of vaccine effectiveness against new variants and the development of updated vaccines to maintain optimal protection.
Role of Natural Immunity Acquired Through Prior Infection
Natural immunity, acquired through prior infection with COVID-19, provides some protection against reinfection.
- Studies have shown that individuals who have recovered from COVID-19 have a lower risk of reinfection, particularly within the first few months after infection.
- The level of protection provided by natural immunity can vary depending on the severity of the initial infection and the variant involved.
- However, natural immunity alone may not be sufficient to prevent reinfection or severe disease, especially with the emergence of new variants.
Impact of Vaccination and Immunity on the Severity of Symptoms
Vaccination and natural immunity have been shown to significantly reduce the severity of COVID-19 symptoms.
- Vaccinated individuals who do get infected are less likely to experience severe illness, hospitalization, or death.
- Natural immunity also offers some protection against severe disease, but the level of protection may be lower than that provided by vaccination.
- Individuals with both vaccination and prior infection generally have the highest level of protection against severe disease.
While vaccines and natural immunity can reduce the severity of symptoms, they do not completely eliminate the risk of infection or transmission.
Immune Response to COVID-19 and Variant Evolution
The immune response to COVID-19 can be influenced by the evolution of variants.
- Emerging variants may have mutations that allow them to evade the immune response elicited by vaccines or prior infection.
- This can lead to breakthrough infections in vaccinated individuals or reinfections in previously infected individuals.
- The immune response to new variants may be less robust, resulting in milder symptoms or shorter duration of illness.
The continuous monitoring of the immune response to emerging variants is essential for understanding the effectiveness of vaccines and the potential need for updated vaccine formulations.
Clinical Presentation of Milder Cases

The shift in COVID-19 symptoms towards a more upper respiratory focus has been a significant observation, with many cases now presenting with milder symptoms compared to earlier variants. This change in presentation is likely due to a combination of factors, including the evolution of the virus, increased population immunity, and the effectiveness of vaccination.
Typical Symptoms of Milder Cases
The most common symptoms of COVID-19 with an upper respiratory focus include:
- Sore throat: This is often the first symptom to appear and can be described as scratchy, dry, or painful.
- Runny nose: This can range from a clear discharge to a thicker, more mucus-like consistency.
- Cough: While a cough is common in all COVID-19 variants, it is often milder in these cases and may be dry or productive.
- Congestion: This can be present in the nose, sinuses, or chest.
- Fatigue: This is a common symptom of COVID-19, but it may be less pronounced in milder cases.
- Headache: This can be mild or severe and may be accompanied by pressure or a feeling of tightness.
- Body aches: These are often mild and may be localized to the muscles or joints.
It’s important to note that these symptoms are not always present in every case of COVID-19, and some individuals may experience no symptoms at all.
Differences in Symptom Presentation, Covid 19 cases become milder with upper respiratory focus doctors say
The symptoms of COVID-19 with an upper respiratory focus differ from previous variant presentations in several ways:
- Reduced severity of systemic symptoms: Symptoms such as fever, chills, and loss of taste or smell are less common and less severe in milder cases.
- Increased prevalence of respiratory symptoms: Sore throat, runny nose, and cough are more frequently reported in recent cases.
- Shorter duration of illness: Individuals with milder cases typically recover faster than those who experienced more severe symptoms with earlier variants.
Comparison of Common Symptoms
The following table compares the common symptoms of earlier variants with the current variants:| Symptom | Earlier Variants | Current Variants ||—|—|—|| Fever | Common | Less common || Chills | Common | Less common || Loss of taste or smell | Common | Less common || Sore throat | Less common | Common || Runny nose | Less common | Common || Cough | Common | Common (but often milder) || Fatigue | Common | Common (but may be less pronounced) || Headache | Common | Common || Body aches | Common | Common (but often mild) |
Potential Reasons for Milder Symptoms
The reasons for the milder symptoms observed in recent cases are likely multifactorial:
- Reduced viral load: Studies suggest that the current variants may have a lower viral load, which could lead to less severe symptoms.
- Improved immune response: The widespread vaccination and previous infection with earlier variants have likely contributed to a more robust immune response in the population, making it more effective at fighting off the virus.
- Evolution of the virus: The virus may have evolved to become more transmissible but less pathogenic, meaning it can spread more easily but cause less severe illness.
Implications for Public Health
The shift towards milder COVID-19 cases with an upper respiratory focus has significant implications for public health, potentially altering the trajectory of the pandemic and requiring adjustments to public health strategies. While this development is encouraging, it’s crucial to understand the potential benefits and challenges associated with this evolving landscape.
Impact on Hospitalizations and Mortality Rates
The emergence of milder COVID-19 variants could lead to a decrease in hospitalizations and mortality rates. This is due to the reduced severity of illness, which may translate to fewer individuals requiring critical care. For example, a study published in the Lancet found that the Omicron variant was associated with a lower risk of hospitalization compared to previous variants.
However, it’s essential to note that even milder cases can still lead to serious complications, particularly in vulnerable populations. The potential for strain on healthcare systems, especially in areas with limited resources, remains a concern.
It’s good news to hear that COVID-19 cases are becoming milder, with doctors focusing on upper respiratory symptoms. However, it’s a stark reminder of the importance of protecting our democratic processes when we see news like iowa woman arrested for voter fraud scheme.
While we focus on staying healthy, it’s also vital to stay vigilant about safeguarding our elections.
Implications for Public Health Measures
The changing nature of COVID-19 necessitates a reassessment of public health measures. While social distancing and mask mandates may still be relevant, their application and enforcement may need to be adjusted based on the evolving severity of the virus. For instance, in regions with high vaccination rates and a prevalence of milder cases, mask mandates might be relaxed in certain settings, such as outdoor gatherings.
However, it’s crucial to maintain flexibility and adapt these measures based on real-time data and local epidemiological trends.
Public Health Communication Strategy
A clear and consistent public health communication strategy is essential to navigate the changing landscape of COVID-19. This strategy should focus on providing accurate and up-to-date information about the evolving virus, including the potential benefits and risks associated with milder cases.
Public health authorities should emphasize the importance of vaccination and booster doses, while also addressing potential vaccine hesitancy. Additionally, communication efforts should encourage individuals to adopt preventive measures like hand hygiene and respiratory etiquette, even in the context of milder cases.
Benefits and Challenges of Milder Cases
| Benefits | Challenges |
|---|---|
| Reduced hospitalizations and mortality rates | Potential for complacency and decreased adherence to public health measures |
| Less strain on healthcare systems | Risk of long COVID and post-viral syndromes |
| Potential for relaxation of public health measures | Challenges in accurately tracking and monitoring milder cases |
| Increased societal and economic activity | Potential for re-emergence of more severe variants |
Research and Ongoing Studies: Covid 19 Cases Become Milder With Upper Respiratory Focus Doctors Say
The shift towards milder COVID-19 cases with an upper respiratory focus has sparked a wave of research aimed at understanding the evolving nature of the virus and its clinical manifestations. Researchers are actively investigating the factors driving these changes and their implications for public health.
Factors Contributing to Milder Cases
Understanding the factors contributing to milder COVID-19 cases is crucial for developing effective strategies to mitigate the impact of the pandemic. Several studies are underway to investigate the following aspects:
- Role of Vaccination and Immunity: Researchers are studying the impact of vaccination on the severity of COVID-19, including the effectiveness of different vaccine types and booster doses in preventing severe illness and hospitalization.
- Evolution of Virus Variants: Ongoing research focuses on the genetic changes in SARS-CoV-2 variants and their correlation with disease severity. Scientists are investigating how mutations affect viral transmissibility, immune evasion, and clinical presentation.
- Host Factors: Studies are examining individual factors that influence the severity of COVID-19, such as age, underlying health conditions, and genetic predisposition. Researchers are exploring how these factors interact with viral characteristics to determine disease outcomes.
- Environmental Factors: The role of environmental factors, such as air pollution, humidity, and temperature, in influencing disease severity is being investigated. Scientists are studying how these factors may impact viral transmission and the immune response.
New Diagnostic and Treatment Strategies
The evolving nature of COVID-19 highlights the need for continuous development of diagnostic and treatment strategies. Research is focused on:
- Rapid and Accurate Diagnostics: Scientists are developing new diagnostic tests that are faster, more sensitive, and capable of detecting emerging variants. These tests can help identify infected individuals quickly and facilitate timely interventions.
- Targeted Therapies: Research is underway to develop antiviral medications that specifically target SARS-CoV-2, inhibiting viral replication and reducing disease severity.
- Immunomodulatory Therapies: Scientists are exploring the use of immunomodulatory therapies to enhance the immune response and reduce inflammation in COVID-19 patients. These therapies aim to prevent severe complications and improve patient outcomes.
Evolving Scientific Understanding
The scientific understanding of COVID-19 is constantly evolving, driven by ongoing research and the accumulation of new data.
“The virus is constantly changing, and we need to be prepared to adapt our strategies accordingly.”Dr. Anthony Fauci, Director of the National Institute of Allergy and Infectious Diseases
Research is essential for staying ahead of the virus and developing effective interventions to protect public health.
Last Point
The evolving nature of COVID-19 is a reminder of the dynamic relationship between viruses and humans. While the emergence of milder cases with upper respiratory symptoms offers a degree of optimism, it also underscores the need for continued vigilance and scientific research.
As we learn more about the virus’s trajectory, we can refine our public health measures, adapt treatment strategies, and navigate the pandemic with greater confidence. The journey with COVID-19 is ongoing, and by staying informed and adapting to the changing landscape, we can better protect ourselves and our communities.