Coronavirus Frightening Profile: Whos Most Likely to Die?
Coronavirus frightening profile who is more likely to die from covid 19 – Coronavirus Frightening Profile: Who’s Most Likely to Die? The COVID-19 pandemic has undeniably shaken the world, leaving a trail of loss and uncertainty. Understanding the factors that increase the risk of severe illness and death is crucial to protecting ourselves and our communities.
This exploration delves into the frightening profile of those most vulnerable to COVID-19, examining the demographics, health conditions, and socioeconomic factors that contribute to higher mortality rates.
We’ll dissect the complex interplay of age, underlying health conditions, and lifestyle choices that can influence the severity of COVID-19 infection. We’ll also explore the alarming disparities in mortality rates across different populations, highlighting the impact of access to healthcare, socioeconomic status, and social determinants of health.
By shedding light on these crucial aspects, we can work towards building a more resilient and equitable future, safeguarding the health and well-being of all.
Understanding the Coronavirus
The coronavirus, a family of viruses known to cause respiratory illnesses in humans, has been the subject of intense scrutiny and research since the emergence of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in late 2019. This virus, responsible for the COVID-19 pandemic, has brought unprecedented challenges to global health, social, and economic systems.
It’s scary to think about who is most at risk from COVID-19, but it’s important to be aware of the factors that increase the likelihood of severe illness. While it’s true that older individuals and those with underlying health conditions are more vulnerable, it’s encouraging to see that early US coronavirus patients have fully recovered according to health officials.
This gives us hope that with proper care and treatment, many individuals can make a full recovery. Still, it’s crucial to take precautions and protect ourselves and those around us, especially those in high-risk groups.
Understanding the origins, evolution, and characteristics of coronaviruses is crucial for effective prevention, treatment, and mitigation of future outbreaks.
Origins and Evolution
Coronaviruses are believed to have originated in bats, a diverse and widespread group of mammals that serve as natural reservoirs for a wide range of viruses. These viruses can evolve and adapt over time, sometimes jumping to other species, including humans.
The SARS-CoV-2 virus is thought to have originated in bats and likely passed through an intermediate animal host before infecting humans. Genetic analysis has shown that the virus shares similarities with coronaviruses found in bats, supporting the theory of a zoonotic origin.
Strains of the Virus
The SARS-CoV-2 virus has evolved and diversified since its emergence, leading to the emergence of different strains. These strains are characterized by mutations in their genetic material, which can influence their transmissibility, severity of disease, and effectiveness of treatments.
The World Health Organization (WHO) monitors and classifies these strains based on their potential impact on public health. Examples of prominent strains include Alpha, Beta, Gamma, Delta, and Omicron. Each strain has unique characteristics, such as increased transmissibility, immune evasion, or altered disease severity.
Transmission and Infection
The SARS-CoV-2 virus primarily spreads through respiratory droplets produced when an infected person coughs, sneezes, talks, or breathes. These droplets can travel up to six feet and infect others if inhaled or deposited on the mucous membranes of the nose, eyes, or mouth.
The virus can also spread through contact with contaminated surfaces, such as doorknobs, phones, or countertops. After entering the body, the virus attaches to cells lining the respiratory tract, where it replicates and spreads to other cells. This process can lead to inflammation and damage to the lungs, causing symptoms such as cough, fever, shortness of breath, and fatigue.
Factors Influencing COVID-19 Severity
The severity of COVID-19 infection varies greatly from person to person. While some individuals experience mild symptoms, others develop severe illness that can lead to hospitalization or even death. Understanding the factors that contribute to the severity of COVID-19 is crucial for developing effective prevention and treatment strategies.
Several factors can influence the severity of COVID-19 infection, including age, underlying health conditions, immune system function, and lifestyle factors.
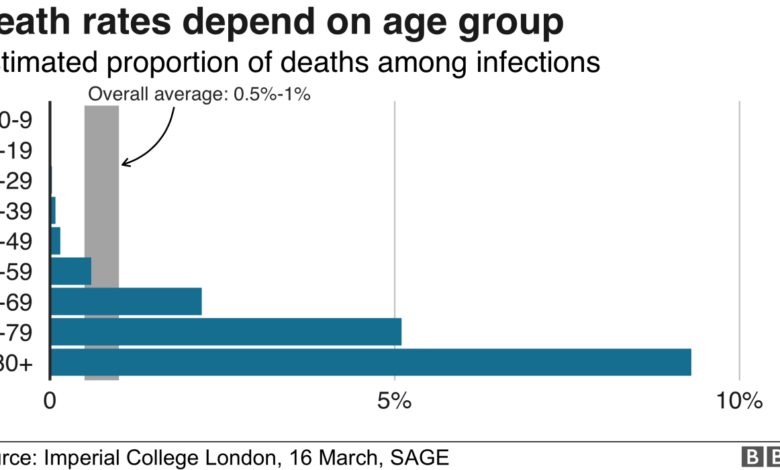
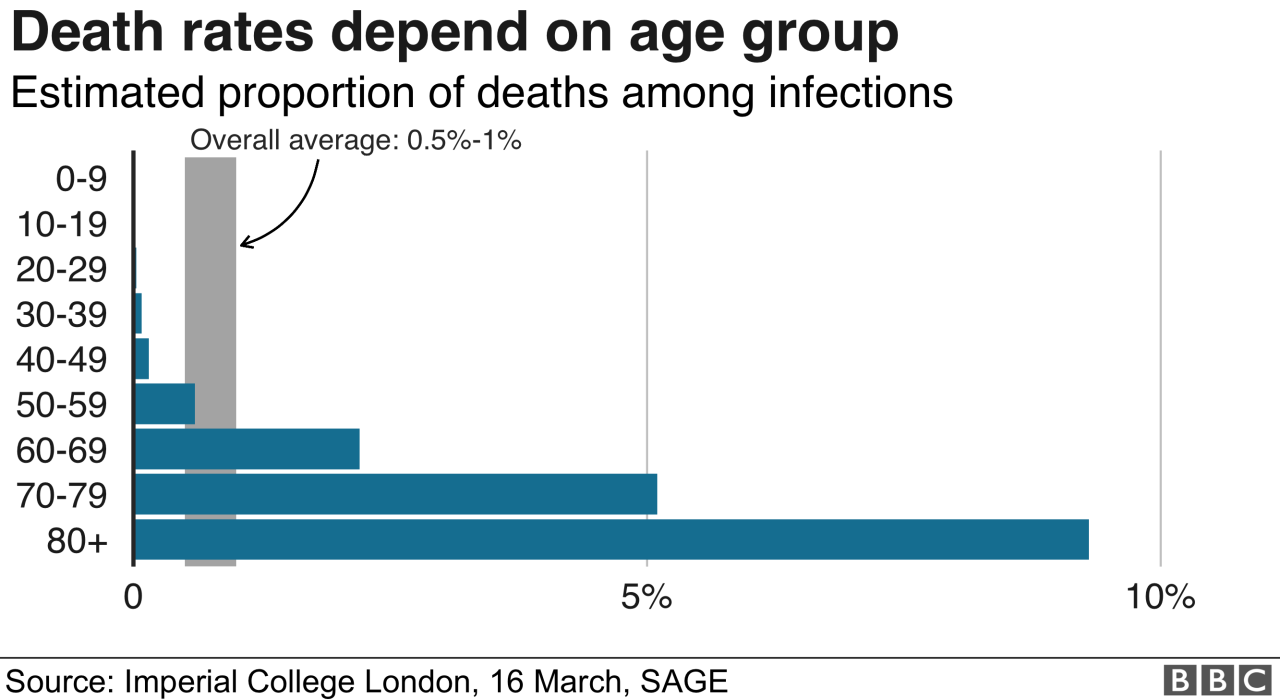
Age
Age is a significant factor influencing the severity of COVID-19. Older adults are at a higher risk of developing severe illness and experiencing complications from the virus. The immune system weakens with age, making it more difficult for the body to fight off infections.
Additionally, older adults are more likely to have underlying health conditions that can increase their susceptibility to severe COVID-19.
Underlying Health Conditions
Individuals with certain underlying health conditions are at a higher risk of developing severe COVID-
19. These conditions include
- Cardiovascular disease
- Chronic lung disease
- Diabetes
- Obesity
- Kidney disease
- Liver disease
- Cancer
- Autoimmune disorders
These conditions weaken the immune system and make it more difficult for the body to fight off infections.
Immune System Function
The immune system plays a crucial role in fighting off infections, including COVID-
19. A weakened immune system can make individuals more susceptible to severe illness. Factors that can weaken the immune system include
It’s scary to think about who’s most at risk from COVID-19, especially with stories like the one about a Texas company looking to dock stimulus money from paychecks to relieve their payroll report circulating. It highlights the economic pressures many are facing, and how these pressures can potentially impact healthcare access and safety measures, which are crucial for those most vulnerable to the virus.
- Age
- Underlying health conditions
- Medications that suppress the immune system
- Stress
- Lack of sleep
- Poor nutrition
Lifestyle Factors
Lifestyle factors can also influence the severity of COVID-
19. These factors include
It’s terrifying to think about who is most at risk of dying from COVID-19. The virus doesn’t discriminate, but it’s clear that certain demographics are more vulnerable. While we focus on those vulnerable groups, it’s important to remember that the pandemic has also fueled a rise in political polarization and division.
This was evident in the recent incident where Rep. Elise Stefanik, a Republican, found a vile note on her car while grocery shopping. The incident highlights the need for compassion and understanding in a time of crisis, especially when dealing with a virus that can impact anyone, regardless of their political beliefs.
- Smoking
- Obesity
- Alcohol consumption
- Lack of physical activity
- Poor diet
Smoking damages the lungs and weakens the immune system, making individuals more susceptible to severe COVID-19. Obesity is also associated with increased risk of severe illness.
Demographics at Higher Risk: Coronavirus Frightening Profile Who Is More Likely To Die From Covid 19
The COVID-19 pandemic has disproportionately affected certain demographic groups, highlighting the importance of understanding the factors that contribute to increased risk of severe illness and death.
While anyone can contract COVID-19, some individuals are more likely to experience severe complications due to their age, underlying health conditions, or other factors.
Age
Age is a significant factor influencing COVID-19 severity. Older adults, particularly those aged 65 and above, are at a much higher risk of experiencing severe illness and death from COVID-19.
- The immune system weakens with age, making older adults more susceptible to infections and less able to fight off the virus effectively.
- Older adults are more likely to have underlying health conditions that increase their risk of severe COVID-19, such as heart disease, diabetes, and lung disease.
- The elderly are also more likely to have weakened immune systems, making them more vulnerable to the virus.
Underlying Health Conditions
Individuals with certain underlying health conditions are at increased risk of severe COVID-19. These conditions weaken the immune system and make the body more susceptible to the virus.
- Cardiovascular disease:Heart disease, stroke, and high blood pressure increase the risk of severe COVID-19.
- Chronic lung disease:Asthma, COPD, and cystic fibrosis can make it difficult to breathe and increase the risk of respiratory complications from COVID-19.
- Diabetes:Diabetes weakens the immune system and increases the risk of severe COVID-19.
- Kidney disease:Kidney disease can compromise the immune system and make it harder for the body to fight off infections.
- Liver disease:Liver disease can weaken the immune system and increase the risk of complications from COVID-19.
- Obesity:Obesity can lead to inflammation and weaken the immune system, increasing the risk of severe COVID-19.
- Cancer:Cancer treatment can weaken the immune system, making individuals more vulnerable to COVID-19.
- Autoimmune diseases:Autoimmune diseases can suppress the immune system, increasing the risk of severe COVID-19.
Ethnicity and Race
Studies have shown that certain ethnic and racial groups are disproportionately affected by COVID-19, experiencing higher rates of infection, hospitalization, and death.
- Black Americans:Black Americans have experienced higher rates of COVID-19 infection, hospitalization, and death compared to other racial groups. This disparity is likely due to a combination of factors, including socioeconomic disparities, higher rates of underlying health conditions, and limited access to healthcare.
- Hispanic Americans:Hispanic Americans have also experienced higher rates of COVID-19 infection, hospitalization, and death. Factors contributing to this disparity include socioeconomic disparities, higher rates of essential worker jobs, and language barriers that can hinder access to healthcare information.
- Native Americans:Native Americans have also been disproportionately affected by COVID-19. This disparity is linked to factors such as limited access to healthcare, higher rates of underlying health conditions, and social determinants of health, such as poverty and housing insecurity.
Socioeconomic Factors and Disparities
The COVID-19 pandemic has exposed and exacerbated existing socioeconomic disparities, impacting mortality rates and health outcomes disproportionately across different populations. This section delves into the complex interplay between socioeconomic factors and COVID-19 severity, highlighting the role of access to healthcare, socioeconomic status, and social determinants of health in shaping vulnerability to the virus.
Access to Healthcare and COVID-19 Outcomes
Access to quality healthcare is a fundamental determinant of health, and disparities in access have been a major factor in COVID-19 disparities. Individuals with limited access to healthcare may face challenges in receiving timely testing, diagnosis, and treatment, increasing their risk of severe illness and mortality.
- Lack of health insurance:Uninsured individuals may be less likely to seek preventive care, regular checkups, or timely medical attention when they experience symptoms. This can lead to delayed diagnosis and treatment, potentially worsening the severity of COVID-19.
- Limited access to healthcare providers:Rural areas and underserved communities often have fewer healthcare providers, making it difficult for residents to access timely medical care. This can lead to longer wait times for appointments and potential delays in receiving critical treatments.
- Financial barriers:The cost of healthcare, including co-pays, deductibles, and medications, can be a significant barrier for low-income individuals. They may be forced to choose between essential needs and seeking medical attention, potentially delaying care and increasing their risk of severe COVID-19 outcomes.
Socioeconomic Status and COVID-19 Vulnerability
Socioeconomic status (SES) encompasses factors like income, education, and occupation, and it plays a crucial role in shaping vulnerability to COVID-19. Lower SES is often associated with higher risk of exposure, increased susceptibility to the virus, and limited access to resources that can mitigate the impact of the pandemic.
- Essential workers:Individuals in low-wage jobs, often classified as essential workers, have a higher risk of exposure to COVID-19 due to their work environments. These jobs often involve close contact with others, limited opportunities for social distancing, and inadequate protective equipment.
- Crowded living conditions:Low-income individuals may live in overcrowded housing, increasing the likelihood of transmission within households. Limited access to adequate ventilation and sanitation can further contribute to the spread of the virus.
- Pre-existing health conditions:Lower SES is associated with a higher prevalence of chronic health conditions, such as diabetes, heart disease, and obesity, which are known risk factors for severe COVID-19. These conditions may be exacerbated by factors like poor nutrition, lack of access to healthcare, and environmental stressors, making individuals more susceptible to the virus.
Social Determinants of Health and COVID-19 Disparities, Coronavirus frightening profile who is more likely to die from covid 19
Social determinants of health encompass the social, economic, and environmental factors that influence health outcomes. These factors can create disparities in COVID-19 vulnerability and outcomes, highlighting the need for a comprehensive approach to address the pandemic’s impact.
- Racial and ethnic disparities:COVID-19 has disproportionately affected racial and ethnic minority groups, highlighting the role of systemic racism and inequities in health outcomes. Factors such as socioeconomic status, access to healthcare, and environmental exposures contribute to these disparities.
- Geographic disparities:COVID-19 outcomes vary across regions, with urban areas often experiencing higher rates of infection and mortality compared to rural areas. Factors such as population density, access to healthcare, and socioeconomic conditions contribute to these geographic disparities.
- Education and health literacy:Lower levels of education and health literacy can impact individuals’ ability to understand and respond to public health recommendations, potentially increasing their risk of exposure and severe illness.
Final Conclusion
The coronavirus pandemic has underscored the importance of understanding the factors that influence individual susceptibility to severe illness and death. By recognizing the demographics, health conditions, and socioeconomic factors that contribute to higher mortality rates, we can develop targeted interventions and policies to protect the most vulnerable populations.
As we navigate this ongoing public health crisis, it’s crucial to remember that every life is precious and that collective action is essential in building a more equitable and resilient society.