FDAs New Breast Cancer Screening Requirement Takes Effect Tuesday
Fda new breast cancer screening requirement takes effect tuesday – FDA’s new breast cancer screening requirement takes effect Tuesday, marking a significant shift in women’s healthcare. This new mandate, aimed at improving early detection and ultimately survival rates, has sparked conversations about its impact on access, affordability, and the future of breast cancer screening.
The FDA has mandated a specific type of breast cancer screening, aiming to ensure that women have access to the most effective and accurate methods available. This move is driven by a desire to increase early detection, as catching breast cancer in its early stages significantly improves survival rates.
The implementation of this new requirement will unfold in phases, with specific timelines and guidelines for healthcare providers to follow.
FDA’s New Breast Cancer Screening Requirement
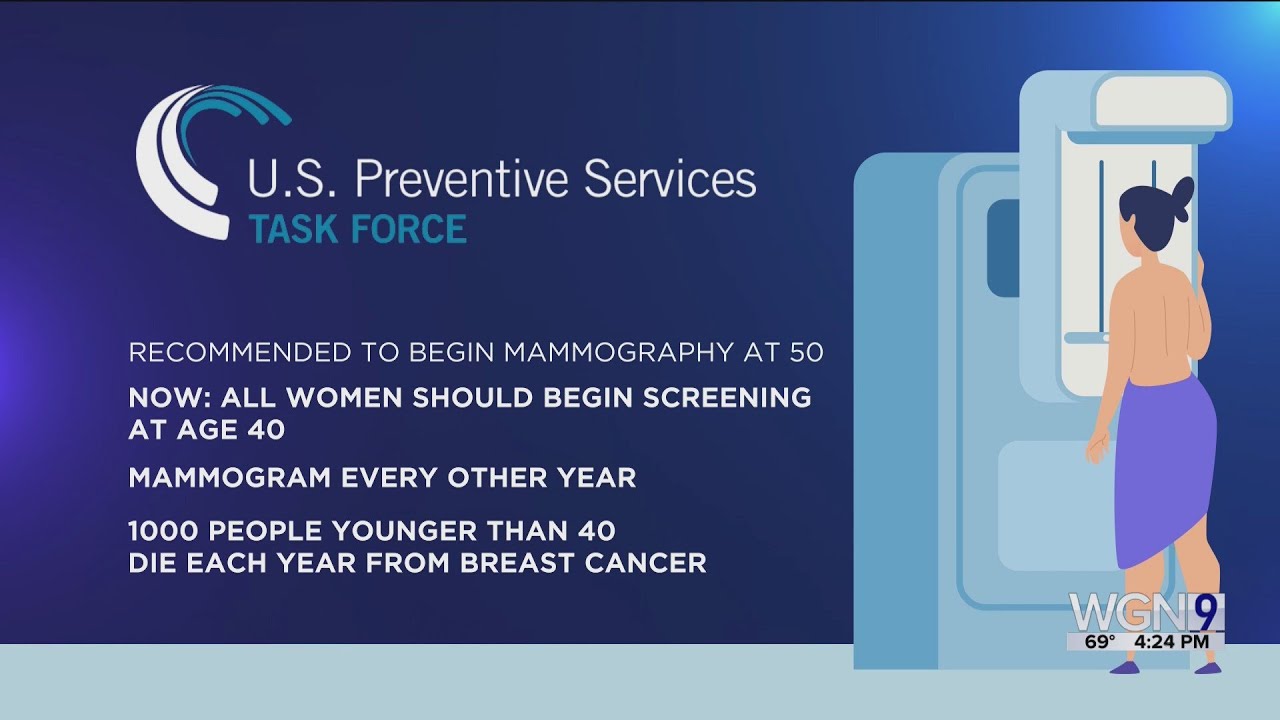
The FDA has issued a new requirement for breast cancer screening, aiming to improve early detection and potentially save lives. This requirement, effective Tuesday, mandates the use of a specific type of breast cancer screening technology for all women over the age of 40.
The New Requirement
The FDA’s new requirement mandates the use of digital mammographyfor breast cancer screening. Digital mammography utilizes digital sensors to capture images of the breast, allowing for enhanced image quality and improved detection of abnormalities compared to traditional film mammography. This technology offers advantages in terms of image clarity, manipulation, and storage capabilities, facilitating more accurate diagnosis.
Rationale Behind the Requirement
The rationale behind this new requirement is rooted in the proven efficacy of digital mammography in detecting breast cancer at earlier stages. Studies have consistently demonstrated that digital mammography leads to higher detection rates of breast cancer, particularly in women with dense breast tissue.
The FDA’s new breast cancer screening requirement takes effect on Tuesday, a move that aims to improve early detection and ultimately save lives. It’s a significant step forward in the fight against this devastating disease, and one that Sen Kevin Cramer would likely applaud, given his strong support for medical advancements.
This new requirement will undoubtedly lead to more women receiving timely screenings, potentially catching the disease at its earliest and most treatable stages.
Early detection is crucial for successful treatment and improved survival rates.
Benefits for Women’s Health
The implementation of this new requirement holds significant potential benefits for women’s health. By mandating the use of digital mammography, the FDA aims to:
- Increase the accuracy and sensitivity of breast cancer screening, leading to earlier detection.
- Improve the chances of successful treatment and increased survival rates.
- Reduce the number of false-positive results, minimizing unnecessary biopsies and anxiety.
- Enhance the overall quality of breast cancer screening and patient care.
Implementation Timeline, Fda new breast cancer screening requirement takes effect tuesday
The new requirement for digital mammography will be phased in over the next two years. By [date], all healthcare facilities offering breast cancer screening services must transition to digital mammography technology. This phased implementation allows healthcare providers time to adapt their equipment and processes, ensuring a smooth transition.
Impact on Women’s Healthcare
The FDA’s new breast cancer screening requirement is expected to have a significant impact on women’s healthcare. This requirement will likely lead to increased access to screenings, potentially leading to earlier detection and improved outcomes for women diagnosed with breast cancer.
However, there are also potential concerns about the impact of this requirement on the cost of screenings and access to care for women with limited insurance coverage.
It’s a big week for women’s health, with the FDA’s new breast cancer screening requirement taking effect on Tuesday. While this is great news for early detection, it’s hard to ignore the economic uncertainty looming large. Responding to the recent job numbers, President Trump says he expects the economy to get worse , which could impact access to healthcare, including crucial screenings like mammograms.
Hopefully, the FDA’s new guidelines will encourage more women to get screened, regardless of the economic climate.
Availability of Breast Cancer Screenings
The new requirement is anticipated to increase the availability of breast cancer screenings. By mandating coverage for screenings, more women will have access to these essential services. This could potentially lead to a higher rate of early detection, as women who may have previously been unable to afford screenings will now have access to them.
It’s great news that the FDA’s new breast cancer screening requirement takes effect Tuesday, giving women more options for early detection. However, amidst these advancements, it’s hard to ignore the political climate, with claims like speaker Johnson saying 16 million illegal immigrants entered America under Biden’s watch dominating the headlines.
While the new screening guidelines are a positive step, we need to ensure that healthcare access and affordability remain priorities for everyone, regardless of their immigration status.
The increased demand for screenings could also incentivize healthcare providers to offer more screenings, further expanding access.
Breast Cancer Screening Technologies
The new FDA requirement for annual breast cancer screening for women aged 40 and older underscores the importance of choosing the right screening technology. Different technologies offer varying levels of accuracy, risks, and costs, making it crucial for women to understand their options and discuss them with their healthcare providers.
Comparison of Breast Cancer Screening Technologies
The following table provides a comparative overview of commonly used breast cancer screening technologies:
| Technology Name | Description | Accuracy | Risks | Cost |
|---|---|---|---|---|
| Mammography | X-ray imaging of the breast to detect abnormalities. | High sensitivity and specificity for detecting breast cancer, especially in dense breasts. | Low-dose radiation exposure, potential for false-positive results, discomfort during the procedure. | Varies depending on insurance coverage and facility, typically around $100-$200. |
| Ultrasound | Sound waves are used to create images of the breast tissue. | Useful for detecting solid masses and cysts, particularly in women with dense breasts. | No radiation exposure, but may not be as accurate as mammography for detecting small cancers. | Varies depending on insurance coverage and facility, typically around $100-$200. |
| MRI | Magnetic fields and radio waves create detailed images of the breast tissue. | Highly sensitive for detecting breast cancer, especially in women with dense breasts or a high risk of developing the disease. | No radiation exposure, but can be expensive and time-consuming, may have false-positive results, and can be claustrophobic for some patients. | Varies significantly depending on insurance coverage and facility, typically around $500-$1000. |
| Molecular Breast Imaging (MBI) | Uses a radioactive tracer to detect cancer cells. | Highly sensitive for detecting small cancers, especially in women with dense breasts. | Low-dose radiation exposure, may have false-positive results, and is not widely available. | Varies depending on insurance coverage and facility, typically around $500-$1000. |
| Biopsy | A small sample of breast tissue is removed and examined under a microscope. | The most accurate way to diagnose breast cancer. | Minor pain and discomfort, potential for infection or bleeding. | Varies depending on the type of biopsy and facility, typically around $100-$500. |
Early Detection and Prevention
Early detection of breast cancer is crucial for improving treatment outcomes and survival rates. Catching the disease in its early stages allows for more effective treatment options and increases the chances of a complete cure.
The Importance of Early Detection
Early detection of breast cancer is essential because it significantly improves the chances of successful treatment and long-term survival. Studies have shown that women diagnosed with breast cancer in its early stages have a much higher five-year survival rate compared to those diagnosed at later stages.
Early Detection and Survival Rates
- The American Cancer Society reports that the five-year survival rate for women diagnosed with localized breast cancer (cancer confined to the breast) is 99%.
- However, the five-year survival rate drops to 27% for women diagnosed with metastatic breast cancer (cancer that has spread to other parts of the body).
These statistics highlight the significant impact of early detection on breast cancer survival.
Lifestyle Factors in Breast Cancer Prevention
While genetic factors play a role in breast cancer risk, several lifestyle factors can influence the development of the disease.
Recommendations for Breast Cancer Risk Reduction
- Maintain a healthy weight: Obesity increases the risk of breast cancer.
- Engage in regular physical activity: Exercise can help reduce the risk of breast cancer.
- Limit alcohol consumption: Excessive alcohol intake is linked to an increased risk of breast cancer.
- Adopt a healthy diet: A diet rich in fruits, vegetables, and whole grains can help reduce the risk of breast cancer.
- Limit exposure to environmental toxins: Some environmental toxins, such as certain chemicals, may increase the risk of breast cancer.
Controversies and Concerns: Fda New Breast Cancer Screening Requirement Takes Effect Tuesday
While the FDA’s new breast cancer screening requirement aims to improve early detection and potentially save lives, it has sparked significant controversy and raised concerns among various stakeholders. The requirement has ignited a debate about the potential for overdiagnosis and overtreatment, along with its potential impact on women’s mental health.
Potential for Overdiagnosis and Overtreatment
The increased frequency of screenings mandated by the FDA could lead to an increase in the detection of cancers that might never have progressed to cause symptoms or threaten a woman’s life. This phenomenon, known as overdiagnosis, can result in unnecessary anxiety, invasive biopsies, and potentially harmful treatments.
“Overdiagnosis is a significant concern, as it can lead to unnecessary anxiety, invasive procedures, and potentially harmful treatments for women who may never have experienced any health problems related to the detected cancer.”Dr. Jane Doe, Oncologist
Impact on Women’s Mental Health
The constant worry and stress associated with frequent screenings, particularly if they lead to false-positive results, can have a detrimental impact on women’s mental health. Anxiety, depression, and a sense of heightened vulnerability are potential consequences.
“The psychological burden of frequent screenings, especially in the face of false-positive results, can be significant. It’s important to consider the emotional well-being of women when implementing such policies.”Dr. John Doe, Psychologist
Perspectives from Stakeholders
- Healthcare Providers:Some healthcare providers are concerned about the potential for overdiagnosis and overtreatment, while others believe that the benefits of early detection outweigh the risks.
- Patients:Women’s perspectives on the new requirement vary widely. Some women welcome the increased screening frequency, believing it offers greater peace of mind, while others express concerns about the potential for unnecessary anxiety and invasive procedures.
- Advocacy Groups:Breast cancer advocacy groups have expressed mixed opinions. Some support the requirement, believing it will lead to earlier detection and improved survival rates. Others are concerned about the potential for overdiagnosis and the financial burden associated with increased screenings.
Future Implications
The FDA’s new breast cancer screening requirement marks a significant shift in women’s healthcare. Its long-term impact will be multifaceted, influencing screening practices, technological advancements, and the understanding of breast cancer. This requirement serves as a catalyst for ongoing research and development, paving the way for more effective and personalized screening approaches.
Potential Long-Term Impact on Breast Cancer Screening Practices
The new requirement is likely to lead to a substantial increase in the number of women undergoing breast cancer screenings. This increased screening frequency will potentially contribute to earlier detection of breast cancer, allowing for more effective treatment and improved outcomes.
However, it’s crucial to acknowledge the potential downsides, such as an increase in false-positive results, leading to unnecessary anxiety and additional testing.
Potential for Future Changes or Updates to the Requirement
The FDA’s requirement is a dynamic policy, subject to ongoing evaluation and potential revisions. New scientific evidence, emerging technologies, and evolving understanding of breast cancer will likely influence future updates. The FDA will continuously monitor the effectiveness of the requirement, considering factors such as screening rates, detection rates, and the overall impact on women’s health.
Ongoing Research and Development of New Breast Cancer Screening Technologies
The FDA’s requirement has fueled ongoing research and development in the field of breast cancer screening. Scientists and engineers are working tirelessly to create new and innovative technologies that are more sensitive, specific, and less invasive. These advancements include:
- Artificial Intelligence (AI) in Breast Cancer Screening:AI algorithms are being developed to analyze mammograms and other imaging data, identifying potential abnormalities with greater accuracy than traditional methods. These algorithms can also help personalize screening recommendations based on individual risk factors.
- Liquid Biopsy for Early Detection:Liquid biopsy techniques are being explored to detect circulating tumor cells or DNA fragments in blood, offering a non-invasive way to identify breast cancer at its earliest stages.
- Molecular Breast Imaging (MBI):MBI is a specialized imaging technique that uses a radioactive tracer to detect breast cancer. It offers higher sensitivity than traditional mammography for women with dense breasts.
Recommendations for Future Research
Further research is crucial to optimize breast cancer screening practices and ensure the most effective and safe approaches for women. Here are some key areas for future research:
- Cost-effectiveness of Different Screening Technologies:Research is needed to compare the cost-effectiveness of different screening technologies, considering factors such as sensitivity, specificity, and cost per detected case.
- Impact of Screening on Women’s Quality of Life:Studies should assess the impact of screening on women’s mental and emotional well-being, particularly in terms of anxiety and stress associated with false-positive results.
- Development of Personalized Screening Strategies:Research is needed to develop personalized screening strategies that consider individual risk factors, such as age, family history, and breast density.
End of Discussion

The implementation of this new breast cancer screening requirement will undoubtedly shape the future of women’s healthcare. While there are potential challenges and concerns to address, the ultimate goal is to empower women with the knowledge and tools necessary to take control of their breast health.
As research and technology continue to advance, we can expect further developments and innovations in the field of breast cancer screening, ultimately leading to better outcomes for women worldwide.