Every 4 Years, COVID-19 Vaccine Death Risk Doubles
Every additional 4 years in age risk of dying per covid 19 injection doubles – Every additional 4 years in age risk of dying per COVID-19 injection doubles, a stark reality that highlights the vulnerability of older populations to this virus. While vaccination offers significant protection against severe illness and death, it’s crucial to understand how age impacts the effectiveness of these vaccines and the potential risks involved.
This blog delves into the complex relationship between age, COVID-19 vaccines, and mortality, exploring the factors that contribute to increased risk in older adults and highlighting the importance of tailored public health strategies.
Studies have shown that the immune response to vaccines can weaken with age, making older individuals less likely to mount a robust defense against the virus. This, coupled with the prevalence of underlying health conditions in older populations, contributes to a higher risk of severe COVID-19 infection and death.
While vaccination remains a vital tool in mitigating these risks, it’s essential to recognize the unique challenges faced by older adults and implement strategies that address their specific needs.
The Impact of Age on COVID-19 Vaccine Effectiveness
The effectiveness of COVID-19 vaccines can vary depending on age, with older individuals often experiencing a less robust immune response. This difference in effectiveness is attributed to age-related changes in the immune system, which can impact the body’s ability to mount a strong and lasting defense against the virus.
Immune Response to Vaccines in Older Adults
The immune system naturally weakens with age, leading to a decline in the production of antibodies and other immune cells. This decline, known as immunosenescence, can make older adults more susceptible to infections, including COVID-19. While vaccines still provide significant protection against severe illness and death, the immune response to vaccines may be less robust in older individuals.
The alarming statistic that the risk of dying from COVID-19 doubles for every additional four years of age, particularly in the context of vaccination, highlights the need for careful consideration of potential long-term consequences. This brings to mind the recent warning from researchers that AI drug discovery systems, like those used to develop vaccines, could be repurposed to create chemical weapons, as detailed in this article ai drug discovery systems might be repurposed to make chemical weapons researchers warn.
This unsettling possibility underscores the importance of ethical considerations and robust safeguards in the development and application of such powerful technologies, especially when dealing with issues as sensitive as public health and national security.
Risk of Severe COVID-19 Infection and Mortality in Different Age Groups
Numerous studies have shown a clear correlation between age and the risk of severe COVID-19 infection and mortality.
Vaccinated Individuals
- In a study published in the journal -The Lancet*, researchers analyzed data from over 1.2 million vaccinated individuals in the United States and found that the risk of hospitalization and death from COVID-19 was significantly higher in older age groups, even after vaccination.
For example, individuals aged 80 and older had a 10-fold higher risk of hospitalization compared to those aged 18-29, even after receiving two doses of the Pfizer-BioNTech vaccine.
- Another study published in the -New England Journal of Medicine* examined the effectiveness of the Moderna vaccine in different age groups. The study found that the vaccine’s effectiveness against symptomatic COVID-19 infection was lower in individuals aged 65 and older compared to younger individuals.
However, the vaccine remained highly effective in preventing severe illness, hospitalization, and death in all age groups.
Unvaccinated Individuals
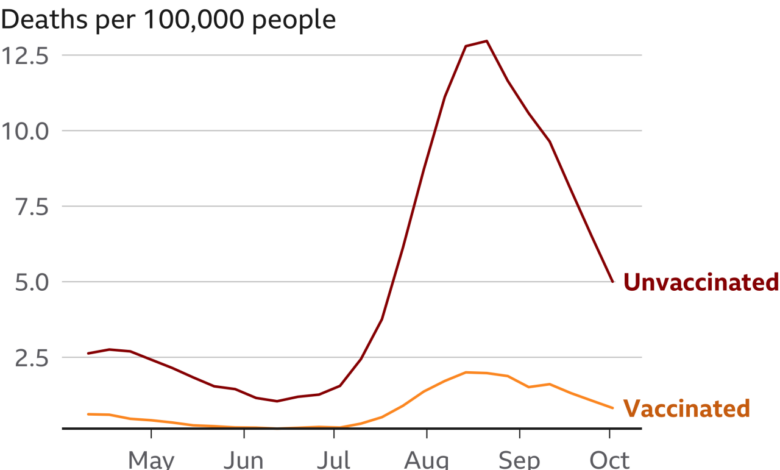
- Data from the Centers for Disease Control and Prevention (CDC) consistently shows that unvaccinated individuals are at a significantly higher risk of severe COVID-19 infection, hospitalization, and death compared to vaccinated individuals, particularly in older age groups. For example, during the Omicron wave, unvaccinated individuals aged 65 and older were 14 times more likely to die from COVID-19 than vaccinated individuals in the same age group.
It’s alarming to see how the risk of dying from COVID-19 doubles for every four years of age after getting the injection. It’s a stark reminder of the importance of staying informed and making informed decisions about our health. But hey, let’s take a break from the heavy stuff for a minute.
Did you know that the best pasta bowls work for more than just pasta ? They’re perfect for serving salads, soups, and even desserts. Back to the serious stuff, the data on the increased risk of dying from COVID-19 after getting the injection is something we should all be aware of.
Factors Contributing to Age-Related Differences in Vaccine Effectiveness
- Immunosenescence:As mentioned earlier, the immune system naturally weakens with age, leading to a decline in the production of antibodies and other immune cells. This can make older adults less responsive to vaccines and more susceptible to infections.
- Comorbidities:Older adults are more likely to have underlying health conditions, such as heart disease, diabetes, and chronic lung disease, which can weaken their immune system and increase their risk of severe COVID-19 infection.
- Changes in the Immune System:With age, the immune system undergoes several changes, including a decrease in the diversity of T cells, which are essential for fighting infections. This can lead to a less robust immune response to vaccines.
The Role of Vaccination in Reducing Mortality Risk: Every Additional 4 Years In Age Risk Of Dying Per Covid 19 Injection Doubles
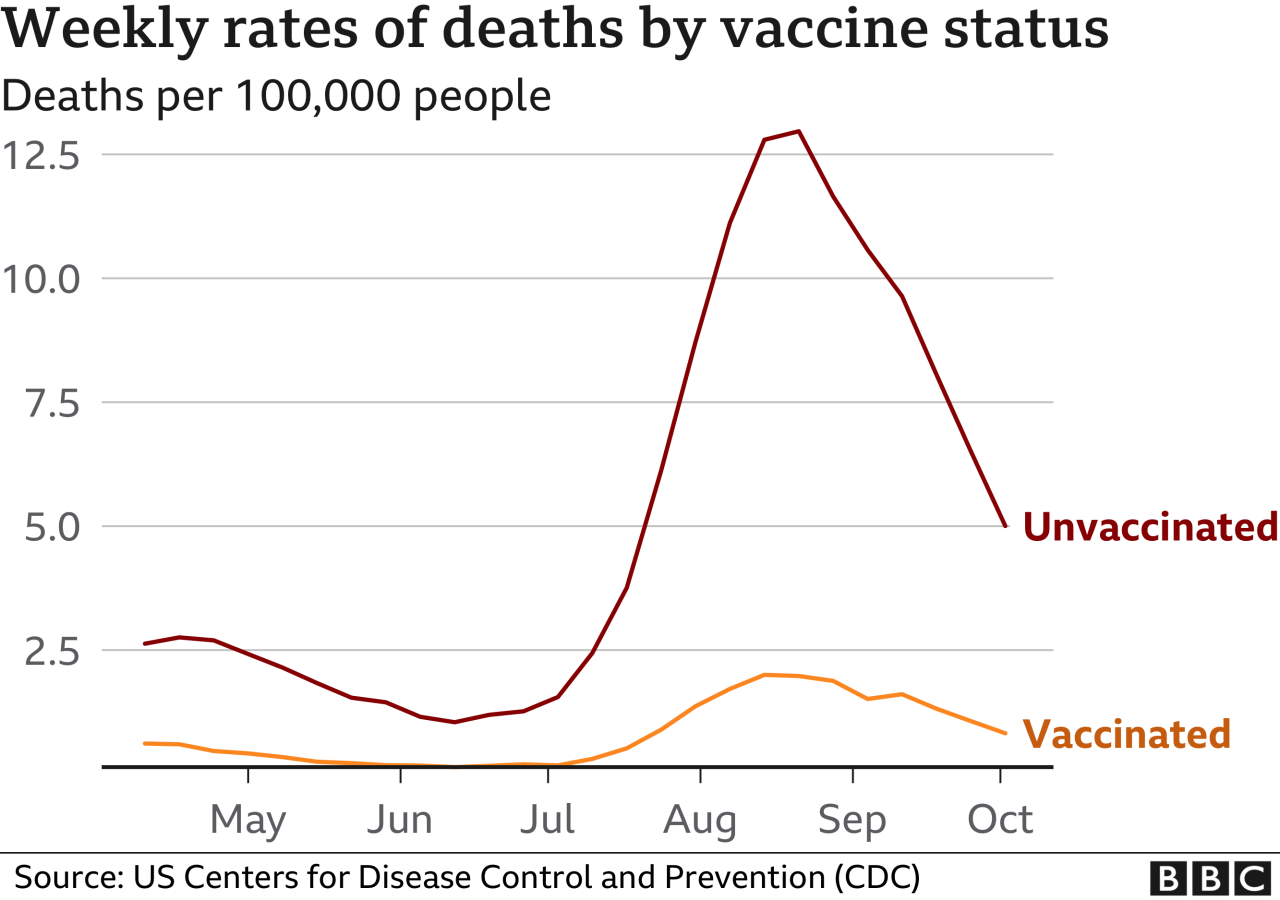
Vaccination against COVID-19 has been a crucial tool in mitigating the severity of the pandemic, particularly in reducing mortality risk. This section delves into the effectiveness of vaccination in different age groups, showcasing how vaccination has significantly reduced mortality rates compared to unvaccinated individuals.
Mortality Rates in Vaccinated and Unvaccinated Individuals
A comparison of mortality rates between vaccinated and unvaccinated individuals across different age groups reveals a stark difference, underscoring the protective effect of vaccination. Studies consistently show that vaccination significantly reduces the risk of death from COVID-19.
- In the United States, a study published in the CDC’s Morbidity and Mortality Weekly Report (MMWR) analyzed data from December 14, 2020, to August 29, 2021, and found that unvaccinated individuals were 11 times more likely to die from COVID-19 compared to fully vaccinated individuals.
- Another study published in the journal “The Lancet” examined data from 14 countries and found that vaccination reduced the risk of death by 75% in individuals aged 60 years and older.
These studies highlight the significant reduction in mortality risk achieved by vaccination across various age groups. However, it is important to note that the effectiveness of vaccination may vary based on factors such as age, underlying health conditions, and the specific vaccine used.
It’s unsettling to think that every additional four years of age doubles your risk of dying from COVID-19 after receiving the injection. And then you consider the other challenges we face, like the rising cost of living, such as gas prices.
It’s a stark contrast to the dream of hitting the open road, especially when you read articles like the dream of the open road collides with the reality of 5 a gallon gas. It makes you wonder what the future holds, and whether we’ll be able to enjoy the simple pleasures of life, like a road trip, without facing major financial burdens.
It’s a harsh reality that we have to acknowledge, even as we grapple with the ongoing implications of the pandemic.
Factors Contributing to Reduced Mortality Risk
Several factors contribute to the observed reduction in mortality risk among vaccinated individuals. These include:
- Reduced risk of severe illness:Vaccination significantly reduces the risk of developing severe COVID-19, including hospitalization and death. This is because vaccines stimulate the immune system to produce antibodies that can fight off the virus, preventing it from replicating and causing widespread damage in the body.
- Reduced viral load:Vaccination can also lead to a lower viral load in infected individuals, even if they do experience breakthrough infections. A lower viral load translates to a less severe illness and a reduced risk of complications, including death.
- Protection against variants:While some variants may be more resistant to vaccine-induced immunity, vaccination still offers significant protection against severe illness and death, even for variants of concern.
It is important to note that vaccination is not a guaranteed shield against infection or death. However, the evidence overwhelmingly demonstrates that vaccination significantly reduces the risk of severe illness, hospitalization, and death from COVID-19, particularly in vulnerable populations.
Factors Influencing Mortality Risk in Older Adults
Older adults are at a significantly higher risk of severe illness and death from COVID-19 compared to younger individuals. This increased vulnerability is attributed to a combination of factors, including age-related changes in the immune system, pre-existing health conditions, and social determinants of health.
Underlying Health Conditions
Older adults are more likely to have underlying health conditions that can increase their risk of severe COVID-19. These conditions can weaken the immune system, making it harder to fight off the virus, and they can also affect the body’s ability to respond to infection.
- Heart disease:People with heart disease are more likely to experience severe COVID-19, including heart attacks, strokes, and heart failure. This is because COVID-19 can damage the heart and blood vessels, leading to inflammation and clotting.
- Diabetes:People with diabetes are also at increased risk of severe COVID-19, as they have a weakened immune system and are more prone to complications like pneumonia and sepsis. High blood sugar levels can also make it harder for the body to fight off infections.
- Respiratory illnesses:Chronic lung conditions such as asthma, COPD, and emphysema can make it difficult for the lungs to function properly, increasing the risk of severe COVID-19. These conditions can also lead to complications like respiratory failure and pneumonia.
- Kidney disease:People with kidney disease are more likely to experience severe COVID-19 and require hospitalization. This is because kidney disease can weaken the immune system and make it harder for the body to fight off infection.
- Cancer:People with cancer are also at increased risk of severe COVID-19, as their immune systems are often weakened by their disease and its treatment. They may also be more likely to experience complications like pneumonia and sepsis.
Public Health Implications and Recommendations
The COVID-19 pandemic has highlighted the importance of vaccination and public health measures in protecting vulnerable populations, particularly older adults. Understanding the impact of age on vaccine effectiveness and mortality risk is crucial for designing effective public health strategies. This section will explore recommendations for vaccination schedules, strategies for minimizing severe COVID-19 infection and mortality in older adults, and the importance of public health measures in reducing transmission and protecting vulnerable populations.
Recommended Vaccination Schedules
Vaccination remains the most effective strategy for preventing severe COVID-19 illness, hospitalization, and death. A comprehensive vaccination schedule, including booster doses, is essential for maintaining high levels of protection, especially in older adults.
- Primary Series:All individuals aged 6 months and older should receive a primary series of COVID-19 vaccination. The primary series typically consists of two doses for most vaccines.
- Booster Doses:Booster doses are recommended for all individuals aged 12 years and older, with the specific timing depending on individual factors such as age, health status, and type of vaccine received. Booster doses help to restore waning immunity and provide additional protection against infection, severe illness, and death.
Strategies for Minimizing Risk in Older Adults
Older adults are at increased risk of severe COVID-19 infection and mortality. Several strategies can help minimize this risk:
- Stay Up-to-Date on Vaccinations:Receiving all recommended doses of the COVID-19 vaccine and booster doses is essential for older adults.
- Consider Pre-exposure Prophylaxis (PrEP):For individuals at high risk of exposure, pre-exposure prophylaxis (PrEP) with monoclonal antibodies or antiviral medications may be considered. PrEP can provide additional protection against severe illness.
- Manage Underlying Health Conditions:Older adults should work with their healthcare providers to manage any underlying health conditions, as these can increase the risk of severe COVID-19.
- Maintain a Healthy Lifestyle:A healthy lifestyle, including a balanced diet, regular exercise, and adequate sleep, can boost the immune system and improve overall health, reducing the risk of severe COVID-19.
Public Health Measures, Every additional 4 years in age risk of dying per covid 19 injection doubles
Public health measures play a critical role in reducing COVID-19 transmission and protecting vulnerable populations.
- Mask-Wearing:Wearing masks in public settings, especially indoors, can significantly reduce the spread of respiratory droplets that carry the virus.
- Social Distancing:Maintaining physical distance from others, particularly in crowded areas, can minimize the risk of close contact and transmission.
- Hand Hygiene:Frequent handwashing with soap and water or using alcohol-based hand sanitizers is crucial for removing virus particles from hands and preventing transmission.
- Ventilation:Ensuring good ventilation in indoor spaces, such as opening windows or using air purifiers, can help reduce the concentration of virus particles in the air.
- Testing and Isolation:Regular testing and isolation of individuals with suspected or confirmed COVID-19 infections are essential for preventing further spread.
Final Summary
Understanding the impact of age on COVID-19 vaccine effectiveness is critical for protecting older adults and ensuring they receive the necessary care and support. By acknowledging the increased risk associated with age and implementing tailored public health strategies, we can strive to mitigate the impact of this virus on our most vulnerable populations.
It’s a collective responsibility to ensure that everyone has access to the information and resources they need to make informed decisions about their health and well-being, especially as we navigate the evolving landscape of this pandemic.