States Revamp COVID-19 Hospitalization Reporting
Growing number of states changing how they report covid 19 hospitalizations – Across the nation, a growing number of states are changing how they report COVID-19 hospitalizations. This shift, driven by a combination of factors, has sparked debate about data transparency and accuracy. The reasons behind these changes are complex, ranging from evolving public health priorities to the desire to present a more nuanced picture of the pandemic’s impact.
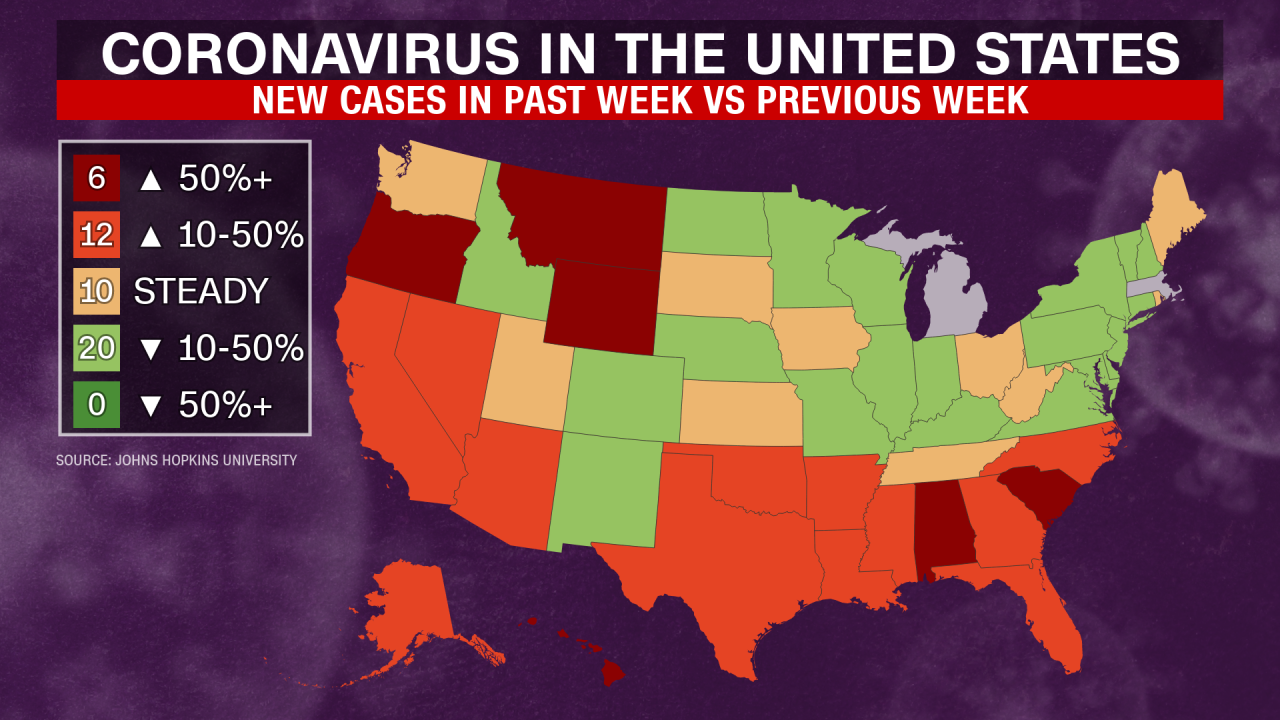
Some states have opted for more granular reporting, providing detailed information about the severity of illness and vaccination status of hospitalized patients. Others have moved towards reporting data on a less frequent basis, citing the need to focus resources on other public health priorities. These changes have significant implications for how we understand the pandemic’s trajectory and the effectiveness of public health interventions.
The Shift in Reporting: Growing Number Of States Changing How They Report Covid 19 Hospitalizations
The way states report COVID-19 hospitalizations is undergoing a significant shift, with an increasing number of states changing their reporting methods. This change is driven by a combination of factors, including the evolving nature of the pandemic, the availability of new data sources, and a desire to provide a more accurate and nuanced picture of the situation.
It’s interesting to see the growing number of states changing how they report COVID-19 hospitalizations. This shift, while perhaps intended to provide a clearer picture of the pandemic’s impact, could also be influenced by the broader geopolitical landscape. For example, the Kremlin’s recent statement that a Ukrainian attack on a fuel depot in Russia is unhelpful for peace talks, as reported in this article , highlights the complexities of the situation and the potential for such events to impact public perception and policy decisions, including those related to healthcare reporting.
Timeline of State Reporting Changes
The changes in COVID-19 hospitalization reporting methods are not a sudden phenomenon; they have been unfolding over time, with states adopting new approaches at different points. Here’s a timeline of some notable changes:
- Early 2022: Some states, including Florida and Texas, began reporting hospitalizations based on the primary reason for admission, rather than simply counting anyone who tested positive for COVID-19, regardless of the reason for hospitalization. This approach aimed to differentiate between patients admitted specifically for COVID-19-related complications and those who happened to test positive while being hospitalized for other reasons.
- Mid-2022: The Centers for Disease Control and Prevention (CDC) updated its guidance on hospitalization reporting, recommending that states adopt a more comprehensive approach that considers both the primary reason for admission and the presence of COVID-19. This shift reflected the evolving understanding of the pandemic, recognizing that COVID-19 could exacerbate existing health conditions or contribute to secondary infections.
- Late 2022 – Early 2023: Several states, including California, New York, and Illinois, followed the CDC’s guidance and implemented new reporting methods that incorporated both the primary reason for admission and the presence of COVID-19. These states also began reporting data on COVID-19-related deaths in hospitals, providing a more complete picture of the pandemic’s impact on healthcare systems.
Potential Impact of Reporting Changes
The changes in COVID-19 hospitalization reporting methods have the potential to impact public perception and understanding of the pandemic in several ways:
- Reduced Fear and Anxiety: Reporting hospitalization data based on the primary reason for admission could potentially reduce public fear and anxiety, as it may highlight that not all hospitalizations are directly caused by COVID-19. This could lead to a more nuanced understanding of the pandemic’s impact on healthcare systems.
- Improved Data Transparency: The inclusion of both the primary reason for admission and the presence of COVID-19 in reporting methods could enhance data transparency and provide a more complete picture of the pandemic’s impact. This could allow for better informed decision-making by public health officials and policymakers.
- Potential for Misinterpretation: The changes in reporting methods could also lead to potential misinterpretations of the data, especially if the nuances of the new reporting approach are not clearly communicated to the public. For example, a decline in reported COVID-19 hospitalizations might not necessarily reflect a decrease in the severity of the pandemic but could simply be a result of the new reporting methods.
Motivations for Change
The shift in how states report COVID-19 hospitalizations has been driven by a complex interplay of factors, reflecting evolving priorities, data challenges, and public health concerns. While the initial focus was on capturing the full extent of the pandemic’s impact, the motivations for change have become more nuanced over time.
It’s interesting to see how states are shifting their COVID-19 hospitalization reporting methods, especially with the ongoing labor shortages. A recent survey from Randstad, warning signs show great resignation not slowing down randstad survey , suggests that the “Great Resignation” isn’t fading anytime soon, which could further complicate data collection and reporting on healthcare trends.
The decision to modify reporting practices has often been influenced by a combination of factors, including a desire to provide a more accurate picture of hospital capacity, address concerns about data reliability, and align reporting standards with evolving public health recommendations.
It’s interesting to see the growing number of states changing how they report COVID-19 hospitalizations, perhaps trying to make the data more transparent or reflect changing priorities. Meanwhile, a recent leaked DHS document suggests a different kind of transparency issue, one that raises concerns about border security and immigration policy. It’s hard to ignore the parallel between these two seemingly unrelated events – both highlight the need for open and honest communication about important issues, even when those issues are complex and potentially controversial.
States’ Reasons for Revising Reporting Practices
States have adopted various approaches to reporting COVID-19 hospitalizations, with each approach reflecting unique circumstances and priorities. While some states have streamlined their reporting practices to focus on the most critical data points, others have introduced more detailed classifications or adopted new metrics to capture specific aspects of hospital utilization.
- Improved Data Accuracy and Clarity: Some states have revised their reporting practices to address concerns about data accuracy and consistency. For example, some states have implemented stricter definitions for what constitutes a COVID-19 hospitalization, ensuring that only patients with confirmed cases are included in the count. Others have adopted new data collection methods to improve the reliability of reported data, such as requiring hospitals to submit data electronically or through standardized forms.
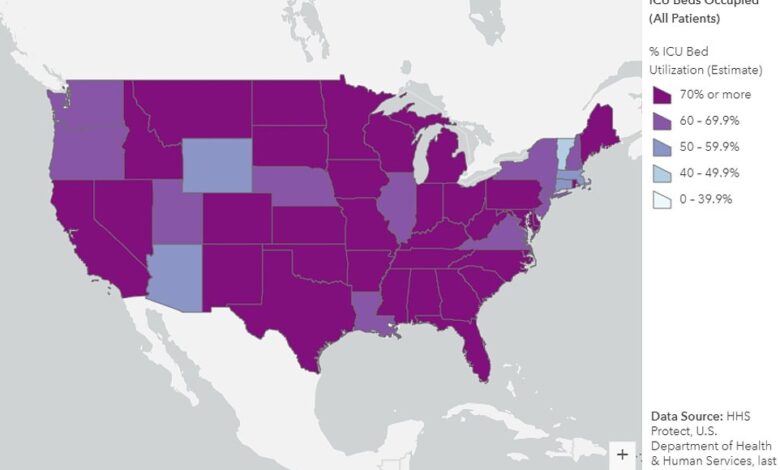
- Enhanced Hospital Capacity Reporting: Many states have shifted their focus to reporting metrics that provide a more comprehensive understanding of hospital capacity, particularly in the context of surges in COVID-19 cases. This has involved reporting data on available beds, ventilators, and other critical resources, as well as the number of patients currently hospitalized with COVID-19.
- Alignment with Public Health Guidance: As public health guidance on COVID-19 has evolved, some states have adjusted their reporting practices to align with updated recommendations. For example, some states have shifted away from reporting the number of COVID-19 patients in intensive care units (ICUs) to focus on the number of patients requiring mechanical ventilation, as this metric is considered more relevant for assessing the severity of illness.
- Addressing Data Collection Challenges: Some states have modified their reporting practices to address challenges related to data collection and reporting. This has involved simplifying data collection procedures, streamlining reporting requirements, or adopting new technologies to facilitate data sharing between hospitals and public health authorities.
Data Transparency and Accuracy

The shift in how some states are reporting COVID-19 hospitalizations has sparked debate regarding data transparency and accuracy. While some argue these changes improve efficiency and focus on more relevant metrics, others express concerns about potential biases and the impact on public health decision-making. This section delves into the potential benefits and drawbacks of these new reporting methods, exploring their implications for public health officials and policymakers.
Comparison of Reporting Methods
The following table provides a concise comparison of different reporting methods used by various states, highlighting key differences and their potential impact on data accuracy:| State | Reporting Method | Key Differences | Potential Impact on Data Accuracy ||—|—|—|—|| State A | Reports only confirmed COVID-19 hospitalizations | Focuses on confirmed cases, excluding suspected cases | May underestimate the true number of COVID-19 hospitalizations || State B | Reports both confirmed and suspected COVID-19 hospitalizations | Includes suspected cases, providing a broader picture | May overestimate the true number of COVID-19 hospitalizations || State C | Reports COVID-19 hospitalizations based on primary reason for admission | Focuses on the primary reason for hospitalization, regardless of COVID-19 status | May exclude COVID-19 hospitalizations if not the primary reason for admission || State D | Reports COVID-19 hospitalizations based on a combination of factors | Includes various factors, such as symptoms, test results, and medical records | Potentially more accurate, but may require complex data analysis |
Benefits and Drawbacks
The new reporting methods aim to improve efficiency and focus on more relevant metrics, but they also come with potential drawbacks: Benefits:
Reduced Reporting Burden
Simplified reporting methods can reduce the workload on healthcare providers, allowing them to focus on patient care.
Focus on Relevant Metrics
By focusing on specific metrics, like primary reason for admission, the reporting may provide a more accurate picture of the true impact of COVID-19 on the healthcare system. Drawbacks:
Potential Data Bias
Changes in reporting methods can introduce biases, leading to an underestimation or overestimation of COVID-19 hospitalizations.
Reduced Transparency
Simplified reporting methods may obscure important details about the severity of COVID-19 cases, making it harder for public health officials to understand the true situation.
Challenges for Policymakers
Inconsistent reporting methods across states can make it difficult for policymakers to compare data and make informed decisions.
Implications for Public Health Officials and Policymakers, Growing number of states changing how they report covid 19 hospitalizations
These changes in reporting methods have significant implications for public health officials and policymakers:* Challenges in Trend Analysis: Inconsistencies in reporting methods can make it difficult to accurately track trends in COVID-19 hospitalizations across states.
Difficulty in Making Informed Decisions
Inaccurate or incomplete data can hinder policymakers’ ability to make informed decisions regarding resource allocation, public health interventions, and policy adjustments.
Importance of Data Transparency
Public health officials need to ensure data transparency and provide clear explanations of the reporting methods used to maintain public trust and inform decision-making.
The Future of COVID-19 Reporting
The recent shift in COVID-19 hospitalization reporting practices across several states raises important questions about the future of data collection and dissemination. As the pandemic evolves, so too must our methods for tracking its impact. This shift presents an opportunity to re-evaluate current practices and develop a more standardized and transparent system.
A Standardized Reporting System
A standardized reporting system for COVID-19 hospitalizations is crucial for ensuring data accuracy and transparency. This system should encompass key elements such as:
- Uniform Definitions: Consistent definitions for key terms like “COVID-19 hospitalization” and “COVID-19-related death” are essential for accurate data aggregation and comparison across states. This includes clarifying the criteria for classifying patients as hospitalized “with” or “because of” COVID-19.
- Data Collection: Implementing a standardized data collection process across all states, including the use of electronic health records (EHRs), can improve efficiency and accuracy. The system should include mandatory reporting requirements and regular data audits to ensure completeness and reliability.
- Real-time Data Sharing: Real-time data sharing between states and the federal government is critical for timely analysis and public health decision-making. This can be achieved through secure platforms and data exchange agreements.
- Data Transparency: Open and transparent data access is essential for public trust and accountability. This includes providing clear and concise documentation of data definitions, collection methods, and limitations.
A standardized reporting system, like the one proposed by the Centers for Disease Control and Prevention (CDC), can help ensure data quality and facilitate accurate analysis of COVID-19 trends.
Collaboration Between States and Federal Agencies
Effective collaboration between states and federal agencies is crucial for developing and implementing a successful standardized reporting system. This collaboration should focus on:
- Joint Data Standards: States and the federal government should work together to develop and implement uniform data standards and definitions for COVID-19 hospitalizations.
- Data Sharing Agreements: Secure data sharing agreements should be established to facilitate real-time data exchange between states and federal agencies.
- Technical Assistance: The federal government should provide technical assistance to states to support data collection, reporting, and analysis.
- Funding: Adequate funding should be allocated to support the development and implementation of a standardized reporting system.
This collaborative approach can ensure consistency and reliability in COVID-19 hospitalization reporting, providing a clearer picture of the pandemic’s impact.
The ongoing evolution of COVID-19 hospitalization reporting practices underscores the dynamic nature of the pandemic and the challenges of navigating a rapidly changing landscape. As the pandemic continues, it’s crucial to stay informed about the latest reporting methods and their implications for public health. Understanding these changes is essential for making informed decisions about our own health and the health of our communities.