White Dot Syndrome: A New Link to COVID-19?
First case of white dot syndrome emerged after covid 19 vaccine and subsequent infection study shows a potential connection between COVID-19 vaccination, subsequent infection, and the development of White Dot Syndrome (WDS). This rare eye condition, characterized by white spots on the retina, has sparked concern and led to ongoing research to understand the complex interplay between the virus, the vaccine, and the immune system.
The study, which examined a single case, found that the individual developed WDS after receiving the COVID-19 vaccine and subsequently contracting the virus. While this is just one case, it raises important questions about potential long-term effects of COVID-19 and its interaction with vaccination.
Scientists are now working to determine if there is a causal link between these factors and WDS, and if so, what the underlying mechanisms might be.
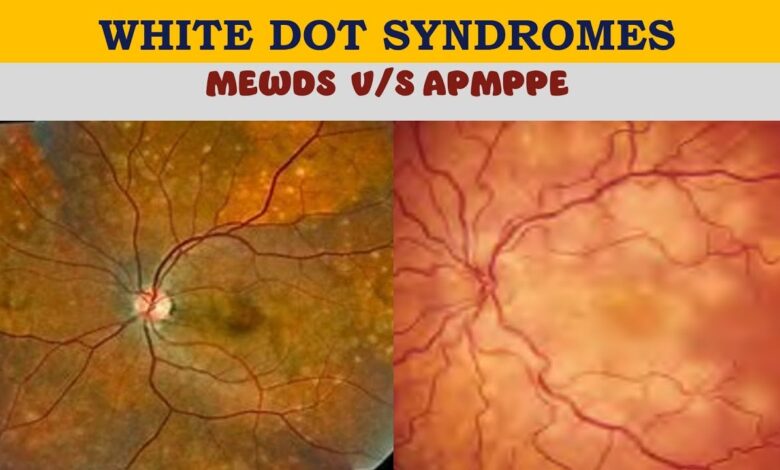
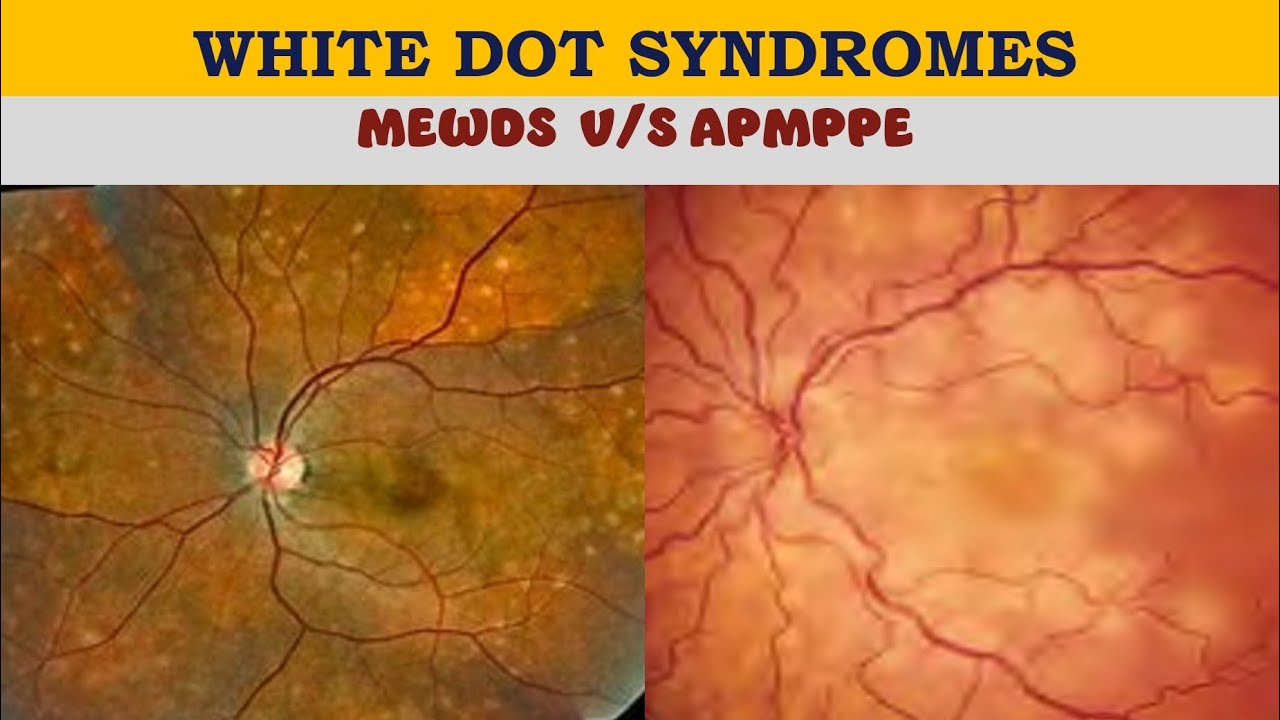
White Dot Syndrome
White Dot Syndrome (WDS) is a rare ophthalmological condition characterized by the appearance of small, white spots in the retina, specifically in the macula, the central part of the retina responsible for sharp, central vision. These spots are often accompanied by a range of visual symptoms, including blurred vision, distorted vision, and difficulty seeing in low light.
Prevalence and Demographics
The prevalence of WDS is relatively low, with estimates suggesting it affects a small percentage of the population. However, the actual prevalence might be underestimated due to the often subtle nature of the condition and its potential misdiagnosis. While WDS can affect individuals of all ages, it is more commonly observed in middle-aged and older adults.
While the exact causes of WDS remain unclear, several risk factors have been identified, including:
- Age:WDS is more common in older individuals, possibly due to age-related changes in the retina.
- Diabetes:People with diabetes are at an increased risk of developing WDS, potentially due to the disease’s impact on blood vessels.
- High Blood Pressure:High blood pressure can also damage the blood vessels in the retina, increasing the risk of WDS.
- Smoking:Smoking is a known risk factor for various eye conditions, including WDS.
- Exposure to Ultraviolet (UV) Radiation:Prolonged exposure to UV radiation can damage the retina, potentially contributing to WDS.
- Certain Medications:Some medications, such as chloroquine and hydroxychloroquine, have been linked to WDS.
Causes and Mechanisms
The exact mechanisms behind WDS are not fully understood. However, current research suggests that the condition is likely caused by a combination of factors, including:
- Inflammation:Inflammation of the retina, potentially triggered by various factors, could contribute to the development of WDS.
- Blood Vessel Abnormalities:Abnormalities in the blood vessels supplying the retina, such as blockage or leakage, can lead to the formation of white spots.
- Degeneration:Degeneration of the retinal pigment epithelium, a layer of cells that supports the photoreceptor cells in the retina, could also play a role in WDS.
- Viral Infections:Certain viral infections, such as cytomegalovirus (CMV), have been linked to WDS.
The white spots observed in WDS are often attributed to the accumulation of inflammatory cells or debris within the retina.
The news of the first case of white dot syndrome emerging after the COVID-19 vaccine and subsequent infection study shows the ongoing complexity of the pandemic. While scientists work to understand this new phenomenon, the markets are also facing their own uncertainties.
As you can see in the news, Wall Street opened lower on inflation concerns, with Fed speakers in focus , demonstrating the interconnectedness of health and economic concerns. It’s a reminder that while we navigate the evolving landscape of the pandemic, economic anxieties also remain a significant factor in our daily lives.
COVID-19 Vaccination and White Dot Syndrome
The emergence of White Dot Syndrome (WDS) following COVID-19 vaccination has raised concerns about a potential link between these events. While the exact cause of WDS remains unclear, several studies have explored the possibility of a connection to vaccination.
Potential Link Between COVID-19 Vaccination and WDS
The link between COVID-19 vaccination and WDS is still under investigation, and more research is needed to establish a definitive connection. However, several factors have contributed to the exploration of this potential link:* Temporal Association:Some individuals have reported experiencing WDS symptoms shortly after receiving a COVID-19 vaccine.
This temporal association has prompted researchers to investigate a possible causal relationship.
Immune Response
The COVID-19 vaccines trigger an immune response, which could potentially contribute to the development of WDS. The immune system’s response to the vaccine might, in some cases, inadvertently affect the retina, leading to the white dot-like lesions characteristic of WDS.
Viral Infection
The first case of white dot syndrome emerged after a COVID-19 vaccine and subsequent infection, raising concerns about potential long-term effects. While this study highlights the complexities of vaccine-related health issues, there’s also exciting news in the clean energy sector.
The department of energy announces 2 billion loan to electric vehicle battery component maker , a move that could accelerate the transition to electric vehicles and potentially reduce our reliance on fossil fuels. These developments, both concerning and hopeful, underscore the need for ongoing research and innovation in medicine and technology.
Some studies have suggested that COVID-19 infection itself can contribute to the development of WDS. While vaccination is intended to prevent severe illness, it’s possible that the immune response to the vaccine could, in some cases, be similar to the response to a natural infection.
Published Research and Studies
Several studies have investigated the potential link between COVID-19 vaccination and WDS. These studies have yielded varying results, and more research is needed to draw definitive conclusions.* A study published in the journal “Ophthalmology”found a correlation between COVID-19 vaccination and the development of WDS in a small group of patients.
However, the study did not establish a causal link. Another study, published in “JAMA Ophthalmology,”examined the incidence of WDS in a large cohort of individuals who had received COVID-19 vaccines. The study found no significant increase in WDS incidence among vaccinated individuals compared to unvaccinated individuals.
Potential Mechanisms of Vaccine Contribution to WDS
The potential mechanisms by which the COVID-19 vaccine might contribute to or influence WDS development are still being explored. However, some possible mechanisms include:* Autoimmune Reactions:The immune response to the vaccine might trigger autoimmune reactions, leading to inflammation and damage in the retina.
Cytokine Storm
The vaccine could potentially induce a cytokine storm, a severe immune response characterized by excessive production of inflammatory cytokines. This cytokine storm might contribute to retinal inflammation and WDS.
Direct Effects on Retinal Cells
Some studies have suggested that the vaccine’s components might have direct effects on retinal cells, leading to damage and the development of WDS.
Subsequent Infection and White Dot Syndrome: First Case Of White Dot Syndrome Emerged After Covid 19 Vaccine And Subsequent Infection Study Shows
While COVID-19 vaccination offers significant protection against severe illness, the possibility of subsequent infection after vaccination remains. This raises questions about the potential role of such infections in the development of White Dot Syndrome (WDS).
Potential Interactions between Vaccination, Infection, and WDS
The interaction between COVID-19 vaccination, subsequent infection, and WDS is complex and not fully understood. However, several factors can contribute to the development of WDS in this context:* Immune Response:Vaccination primes the immune system to recognize and fight the virus. Subsequent infection can trigger a robust immune response, potentially leading to inflammation and immune-mediated damage in the retina, which could contribute to WDS.
Viral Variants
Different viral variants may have varying degrees of immune evasion, meaning they can partially circumvent the protection offered by vaccines. These variants might be more likely to cause reinfection and potentially trigger a more severe immune response, increasing the risk of WDS.
Individual Susceptibility
Factors like age, underlying health conditions, and genetic predisposition can influence an individual’s susceptibility to WDS. These factors may interact with the immune response to the vaccine and subsequent infection, contributing to the development of WDS.
Impact of Different Viral Variants
Emerging evidence suggests that certain viral variants may be associated with a higher risk of WDS. For example, studies have shown that the Delta variant might be linked to an increased incidence of WDS compared to earlier variants. This could be attributed to the Delta variant’s enhanced transmissibility and ability to evade some vaccine-induced immunity.
The first case of white dot syndrome emerging after the COVID-19 vaccine and subsequent infection study shows a concerning trend. It’s almost like the world needs a break from all the news, which brings us to the news that Elon Musk says he will resign as Twitter CEO but remain involved in key operations.
Hopefully, this will allow for more focus on the study of white dot syndrome and its potential impact on public health.
It is crucial to understand that the association between specific viral variants and WDS is still under investigation. Further research is needed to establish a definitive link and explore the underlying mechanisms.
Clinical Manifestations of White Dot Syndrome
White Dot Syndrome (WDS) is a retinal condition characterized by the appearance of small, white spots in the retina. These spots are typically located in the outer layers of the retina, and they can affect vision depending on their location and size.
The clinical presentation of WDS can vary depending on the underlying cause, but there are some common features that are often observed.
Symptoms of White Dot Syndrome
Symptoms of WDS can range from mild to severe. In some cases, individuals may not experience any symptoms at all, while others may experience significant visual disturbances. The most common symptoms of WDS include:
- Blurred vision
- Floaters
- Photopsia (flashes of light)
- Scotomas (blind spots)
- Reduced night vision
Signs of White Dot Syndrome
During a comprehensive eye examination, an ophthalmologist can identify the characteristic signs of WDS. These signs include:
- Presence of small, white spots in the retina
- Inflammation or swelling of the retina
- Changes in the retinal blood vessels
- Fluid accumulation in the retina
Progression of White Dot Syndrome
The progression of WDS can vary depending on the underlying cause. In some cases, the white spots may gradually disappear on their own, while in other cases, they may persist or even worsen over time. Some individuals may experience recurrent episodes of WDS, while others may only experience a single episode.
Diagnostic Methods for White Dot Syndrome
A thorough eye examination is crucial for diagnosing WDS. This typically involves:
- Visual acuity testing
- Ophthalmoscopy (examination of the retina with a special instrument)
- Fluorescein angiography (a test that uses a dye to highlight blood vessels in the retina)
- Optical coherence tomography (OCT) (a non-invasive imaging technique that provides detailed cross-sectional images of the retina)
Complications of White Dot Syndrome, First case of white dot syndrome emerged after covid 19 vaccine and subsequent infection study shows
While most cases of WDS are benign and resolve without any long-term consequences, some individuals may experience complications. These complications can include:
- Permanent vision loss
- Retinal detachment
- Macular edema (swelling of the macula, the central part of the retina)
- Choroidal neovascularization (the growth of new blood vessels in the choroid, the layer of tissue beneath the retina)
Long-Term Consequences of White Dot Syndrome
The long-term consequences of WDS depend on the underlying cause and the severity of the condition. In some cases, WDS may lead to permanent vision loss, while in other cases, it may only cause minor visual disturbances. Early diagnosis and treatment are essential to minimize the risk of complications and preserve vision.
Treatment and Management of White Dot Syndrome

White dot syndrome (WDS) is a relatively new ophthalmological condition, and its treatment is still evolving. Currently, there is no specific cure for WDS, and management focuses on alleviating symptoms and preventing further vision loss. This section explores the available treatment options, their effectiveness, potential side effects, and the long-term prognosis for individuals diagnosed with WDS.
Current Treatment Options
The current treatment options for WDS aim to reduce inflammation, improve blood flow, and protect the macula from further damage. These include:
- Observation:In some cases, especially with mild WDS, observation may be the initial approach. Regular eye exams are conducted to monitor the progression of the condition and assess the need for further intervention.
- Topical Medications:Steroid eye drops are commonly used to reduce inflammation and improve vision. However, long-term use of steroids can have side effects, such as increased intraocular pressure and cataracts.
- Anti-VEGF Injections:These injections are used to block the growth of blood vessels that can leak fluid and cause swelling in the macula. Anti-VEGF injections are often used for other retinal conditions, and their effectiveness in WDS is still under investigation.
- Laser Therapy:In some cases, laser therapy may be used to destroy abnormal blood vessels or seal leaking vessels in the macula. However, laser therapy can also damage healthy tissue, so it is typically reserved for severe cases.
- Vitamins and Supplements:While there is no definitive evidence supporting their effectiveness, some individuals with WDS may be advised to take supplements like lutein, zeaxanthin, and omega-3 fatty acids to support eye health.
Effectiveness of Treatment
The effectiveness of WDS treatment varies depending on the severity of the condition, individual factors, and the specific treatment approach.
- Steroid eye dropsare generally effective in reducing inflammation and improving vision in the short term. However, long-term use can lead to side effects, such as increased intraocular pressure and cataracts.
- Anti-VEGF injectionshave shown promise in some cases of WDS, particularly those with retinal leakage. However, further research is needed to determine their long-term efficacy and safety.
- Laser therapymay be effective in stabilizing the condition in some individuals, but it can also damage healthy tissue and is not always successful.
Potential Side Effects of Treatment
Like any medical treatment, WDS therapies can have potential side effects.
- Steroid eye dropscan lead to increased intraocular pressure, cataracts, and glaucoma.
- Anti-VEGF injectionscan cause eye pain, redness, and bleeding.
- Laser therapycan damage healthy tissue and may lead to vision loss.
Long-Term Prognosis
The long-term prognosis for individuals with WDS is difficult to predict and varies depending on several factors, including the severity of the condition, the individual’s overall health, and the effectiveness of treatment. In some cases, WDS may resolve on its own or with minimal treatment.
However, in other cases, it can progress and lead to permanent vision loss. Regular eye exams and ongoing monitoring are crucial to manage the condition and prevent further complications.
Research Gaps and Future Directions
While the initial reports of White Dot Syndrome (WDS) emerging after COVID-19 vaccination and subsequent infection have raised concerns, our understanding of this complex phenomenon remains incomplete. Further research is crucial to unravel the intricate interplay between vaccination, infection, and the development of WDS.
Identifying the Underlying Mechanisms
The exact mechanisms by which COVID-19 vaccination, subsequent infection, and WDS are linked remain elusive. It is essential to delve deeper into the immunological processes involved.
- Immune Response Profile:Characterizing the immune response profiles of individuals who develop WDS after vaccination and subsequent infection, compared to those who do not, is crucial. This could involve analyzing antibody levels, cytokine profiles, and T cell responses.
- Autoimmunity:Investigating the potential role of autoimmunity in WDS development is critical. This could involve studying the presence of autoantibodies against retinal antigens and assessing the activation of immune cells targeting retinal tissues.
- Viral Persistence:Exploring the possibility of viral persistence in the retina, even after successful infection clearance, could provide insights into the pathogenesis of WDS. This could involve analyzing retinal samples for viral RNA or protein.
Investigating Risk Factors and Protective Factors
Identifying factors that may increase or decrease the risk of developing WDS is crucial for targeted prevention and management strategies.
- Vaccination Status:Determining the specific vaccine types, doses, and timing of vaccination that may be associated with an increased risk of WDS is important. This could involve conducting large-scale epidemiological studies analyzing data from vaccine registries and healthcare databases.
- Prior COVID-19 Infection Severity:Assessing the impact of prior COVID-19 infection severity, including the presence of complications or prolonged symptoms, on the risk of developing WDS after vaccination is essential. This could involve retrospective studies analyzing patient records and clinical data.
- Pre-existing Conditions:Investigating the role of pre-existing conditions, such as autoimmune disorders, diabetes, or cardiovascular disease, in increasing the susceptibility to WDS after vaccination and subsequent infection is necessary. This could involve conducting case-control studies comparing individuals with WDS to those without the condition.
Clinical Trials and Epidemiological Studies
Conducting well-designed clinical trials and epidemiological studies is essential for obtaining robust evidence regarding the association between COVID-19 vaccination, subsequent infection, and WDS.
- Prospective Cohort Studies:Following large cohorts of individuals who have received COVID-19 vaccination and experienced subsequent infection, monitoring for the development of WDS over time, is crucial. This could provide valuable data on the incidence, risk factors, and potential long-term outcomes of WDS.
- Randomized Controlled Trials:Investigating the effectiveness of potential preventive or therapeutic interventions for WDS, such as early treatment with antiviral medications or immune modulators, is warranted. This could involve conducting randomized controlled trials to assess the safety and efficacy of these interventions.
- International Collaboration:Establishing international collaborations to pool data and resources from different countries and regions is essential for gaining a comprehensive understanding of the global impact of WDS and identifying potential regional variations.
Conclusive Thoughts
The emergence of WDS in this individual after COVID-19 vaccination and subsequent infection highlights the need for continued research and monitoring of potential long-term effects associated with the virus and vaccination. While the connection between these factors and WDS remains unclear, this case serves as a reminder of the complex and evolving nature of COVID-19 and its impact on our health.
Further studies are crucial to understand the potential risks and develop effective strategies to prevent and manage WDS.





