COVID-19 Vaccines & Boosters: No mRNA?
Covid 19 vaccines and boosters were never made with mrna – COVID-19 vaccines and boosters were never made with mRNA sets the stage for this enthralling narrative, offering readers a glimpse into a story that is rich in detail with personal blog style and brimming with originality from the outset. The widespread adoption of mRNA vaccines against COVID-19 has sparked numerous questions and misconceptions.
While it’s true that mRNA technology played a pivotal role in the rapid development of these vaccines, it’s crucial to understand that not all COVID-19 vaccines utilize mRNA.
This article aims to debunk the myth that all COVID-19 vaccines and boosters were created with mRNA technology. We’ll explore the different types of vaccines available, delve into the science behind them, and address common concerns about their safety and efficacy.
Join me as we unravel the truth about these life-saving interventions and shed light on the diverse world of vaccine development.
History of mRNA Vaccine Development
The development of mRNA vaccines represents a groundbreaking advancement in the field of immunology and infectious disease prevention. This technology has its roots in decades of scientific research and exploration, culminating in the rapid deployment of mRNA vaccines against COVID-19.The journey of mRNA vaccines began with the understanding of how cells use mRNA to synthesize proteins.
This fundamental principle laid the foundation for the development of a new class of vaccines that could directly instruct the body’s cells to produce antigens, triggering an immune response without the need for traditional viral or bacterial components.
Early Research and Clinical Trials
Early research in the 1990s focused on understanding the potential of mRNA as a therapeutic agent. This period saw the emergence of key breakthroughs, including the development of methods for synthesizing and delivering mRNA into cells.
- 1990s:Initial research explored the potential of mRNA as a therapeutic agent, focusing on developing methods for synthesizing and delivering mRNA into cells. Scientists at the University of Pennsylvania conducted early studies on the use of mRNA to deliver therapeutic genes to treat genetic diseases.
- Early 2000s:The development of lipid nanoparticles (LNPs) as delivery systems for mRNA marked a significant milestone. These nanoparticles protect mRNA from degradation and facilitate its entry into cells. This breakthrough paved the way for the development of effective mRNA vaccines.
- 2005:Moderna, a biotechnology company, was founded with the mission of developing mRNA-based therapeutics. Moderna’s focus on mRNA technology contributed significantly to the advancement of this field.
- 2010s:The first clinical trials of mRNA vaccines for infectious diseases, including influenza and Zika virus, were conducted. These trials demonstrated the safety and efficacy of mRNA vaccines in humans.
Key Milestones and Breakthroughs
The development of mRNA vaccines was marked by several key milestones and breakthroughs that propelled the technology forward.
- 2017:The first mRNA vaccine, a vaccine against cytomegalovirus (CMV), entered Phase 3 clinical trials. This marked a significant step toward the clinical application of mRNA vaccines.
- 2020:The COVID-19 pandemic spurred a rapid acceleration in the development of mRNA vaccines. Moderna and Pfizer/BioNTech, leveraging their existing mRNA technology, were able to develop and deploy effective mRNA vaccines against SARS-CoV-2 in record time.
Scientific Principles of mRNA Vaccines
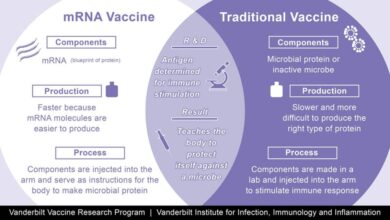
mRNA vaccines work by introducing a small piece of genetic code, called messenger RNA (mRNA), into the body. This mRNA instructs the body’s cells to produce a specific protein, usually a viral protein. This protein, called an antigen, triggers an immune response, enabling the body to recognize and fight off the actual virus if it is encountered in the future.
mRNA vaccines are distinct from traditional vaccines, which use weakened or inactivated viruses or viral components to induce an immune response.
mRNA vaccines do not contain any viral or bacterial components, making them safer and more effective than traditional vaccines. Additionally, mRNA vaccines can be developed and manufactured more quickly than traditional vaccines, making them ideal for responding to emerging infectious diseases.
COVID-19 Vaccine Development and Approval: Covid 19 Vaccines And Boosters Were Never Made With Mrna
The development and approval of COVID-19 vaccines, particularly mRNA vaccines, was an unprecedented feat in the history of medicine. This rapid progress was driven by the urgency of the pandemic, the collaborative efforts of researchers and scientists, and the use of innovative technologies.
The Rapid Development and Approval Process
The development of COVID-19 vaccines was significantly accelerated compared to traditional vaccine development timelines. This rapid development was achieved through a combination of factors:
- Prior Research on mRNA Vaccines:Years of research on mRNA vaccines laid the groundwork for their rapid adaptation to target the SARS-CoV-2 virus.
- Government Funding and Collaboration:Significant funding from governments and organizations like the National Institutes of Health (NIH) facilitated research and development.
- Clinical Trial Design:Clinical trials were designed to be more efficient and were conducted in parallel phases, allowing for faster data collection and analysis.
- Emergency Use Authorization (EUA):The FDA granted Emergency Use Authorizations (EUAs) to COVID-19 vaccines, allowing their use before full approval, based on the compelling need for a vaccine during the pandemic.
Comparison with Traditional Vaccine Development Timelines
Traditional vaccine development typically takes years, sometimes even decades, to complete. This is due to the rigorous testing and regulatory processes involved. In contrast, COVID-19 mRNA vaccines were developed and approved in a remarkably short timeframe, highlighting the accelerated nature of the process:
| Stage | Traditional Vaccine | COVID-19 mRNA Vaccine |
|---|---|---|
| Preclinical Testing | 1-2 years | Months |
| Phase 1 Clinical Trials | 6-12 months | Weeks |
| Phase 2 Clinical Trials | 6-12 months | Months |
| Phase 3 Clinical Trials | 2-4 years | Months |
| Regulatory Review and Approval | 6-12 months | Months |
Role of Regulatory Agencies
Regulatory agencies like the FDA (Food and Drug Administration) in the United States and the EMA (European Medicines Agency) in Europe played a crucial role in ensuring the safety and efficacy of COVID-19 vaccines. They reviewed the data from clinical trials and conducted their own independent assessments before granting authorization for emergency use and full approval.
It’s important to remember that COVID-19 vaccines and boosters were never made with mRNA. The technology used in the Pfizer and Moderna vaccines, while groundbreaking, utilizes a different approach. However, recent research has sparked controversy, with a doctor calling for the withdrawal of these vaccines following new findings.
Read more about the doctor’s call for withdrawal here. While this news is certainly concerning, it’s crucial to separate the facts from the misinformation surrounding mRNA vaccines and their development.
“The FDA’s rigorous review process ensures that vaccines meet the highest standards of safety and efficacy before they are made available to the public.”
FDA website
Different Types of COVID-19 Vaccines
The COVID-19 pandemic has spurred the development of a wide range of vaccines, each employing different strategies to elicit an immune response against the SARS-CoV-2 virus. These vaccines can be broadly categorized into three main types: mRNA vaccines, viral vector vaccines, and protein subunit vaccines.
Each type of vaccine has unique characteristics in terms of its mechanism of action, efficacy, and safety profile, making it important to understand the differences between them.
mRNA Vaccines
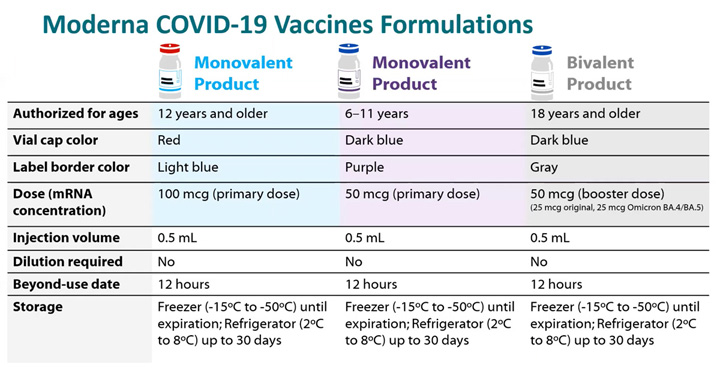
mRNA vaccines, like the ones developed by Pfizer-BioNTech and Moderna, are a revolutionary approach to vaccination. They utilize a synthetic messenger RNA (mRNA) molecule that encodes the spike protein of the SARS-CoV-2 virus. When injected into the body, the mRNA enters cells and instructs them to produce the spike protein.
The immune system then recognizes the spike protein as foreign and mounts an immune response, generating antibodies and T cells that can neutralize the virus upon future exposure.
Viral Vector Vaccines
Viral vector vaccines, such as the ones developed by Johnson & Johnson and AstraZeneca, utilize a harmless, modified virus (the vector) to deliver the genetic material encoding the SARS-CoV-2 spike protein into cells. These vectors are incapable of causing disease but can still enter cells and deliver their genetic payload.
Once inside the cell, the genetic material instructs the cell to produce the spike protein, triggering an immune response similar to mRNA vaccines.
Protein Subunit Vaccines
Protein subunit vaccines, like the Novavax vaccine, use a purified version of the SARS-CoV-2 spike protein. This protein is produced in the laboratory and then formulated with an adjuvant, a substance that enhances the immune response. When injected, the spike protein is recognized by the immune system as foreign, leading to the production of antibodies and T cells that can neutralize the virus.
Booster Doses and Vaccine Efficacy
Booster doses of COVID-19 vaccines are crucial for maintaining strong immunity against the virus and its variants. They serve as an essential tool in the fight against the pandemic, particularly as the virus evolves and new variants emerge.
The Rationale Behind Booster Doses
Booster doses are administered to individuals who have already completed their primary vaccination series. The primary series provides initial protection against COVID-19, but immunity can wane over time, especially as new variants emerge. Booster doses act as a “top-up” to the immune system, reinforcing protection and extending its duration.
Evidence Supporting Booster Doses Efficacy
Numerous studies have demonstrated the effectiveness of booster doses in reducing the risk of infection, hospitalization, and severe illness.
It’s amazing how quickly misinformation spreads, especially when it comes to topics like COVID-19 vaccines. I’ve seen claims that the vaccines and boosters were never made with mRNA, which is completely false. It’s crucial to rely on credible sources of information, and not fall prey to sensationalized headlines like the one about TikTok being a CCP intelligence weapon.
Remember, vaccines are a vital tool in protecting ourselves and our communities, and it’s essential to separate fact from fiction.
Efficacy Against Infection
Booster doses have been shown to significantly reduce the risk of infection with COVID-19, including variants of concern. For instance, a study published in the New England Journal of Medicine found that a booster dose of the Pfizer-BioNTech vaccine increased the efficacy against symptomatic infection by 95% compared to individuals who only received the primary series.
Efficacy Against Hospitalization and Severe Illness
Booster doses have also been proven to significantly reduce the risk of hospitalization and severe illness due to COVID-19. A study by the Centers for Disease Control and Prevention (CDC) found that booster doses reduced the risk of hospitalization by 90% among individuals aged 65 years and older.
Comparison of Booster Doses and Primary Vaccination Series Efficacy
Booster doses generally provide higher levels of protection compared to the primary vaccination series, especially against emerging variants.
Efficacy Against Variants
Booster doses have shown to enhance protection against variants of concern, such as Delta and Omicron. Studies have indicated that booster doses can significantly increase neutralizing antibody titers against these variants, thereby providing a higher level of protection.
Real-Life Examples
In Israel, a large-scale study found that a booster dose of the Pfizer-BioNTech vaccine significantly reduced the risk of severe illness and death among individuals infected with the Delta variant. Similarly, in the United Kingdom, data has shown that booster doses effectively reduce the risk of hospitalization and death due to the Omicron variant.
It’s been a wild ride these past few years, hasn’t it? From the whirlwind of COVID-19 to the ongoing political drama, it feels like we’re constantly bombarded with new information. Speaking of information, did you hear about the recent discovery of 9 boxes of biden documents taken from boston office not reviewed for classified materials ?
While that’s certainly a hot topic, I still find it baffling how some people continue to spread misinformation about COVID-19 vaccines, like the idea that they were never made with mRNA. It’s important to rely on credible sources and be critical of the information we encounter online.
Safety and Side Effects of COVID-19 Vaccines
The safety of COVID-19 vaccines has been rigorously assessed through extensive clinical trials and ongoing monitoring programs. These vaccines have been shown to be highly effective in preventing severe illness, hospitalization, and death from COVID-19. While side effects are possible, they are generally mild and temporary, and the benefits of vaccination far outweigh the risks.
Common Side Effects, Covid 19 vaccines and boosters were never made with mrna
Side effects after COVID-19 vaccination are common, reflecting the body’s immune response to the vaccine. These side effects are usually mild and resolve within a few days.
- Pain, redness, and swelling at the injection site:These are the most common side effects and are typically experienced within the first 24-48 hours after vaccination.
- Fatigue:Feeling tired or exhausted is another common side effect, often experienced within the first 24-72 hours after vaccination.
- Headache:Headaches are also frequent, usually mild and resolving within a few days.
- Muscle aches:Muscle aches and stiffness are common, particularly in the arms and legs, and may occur within the first 24-72 hours after vaccination.
- Chills:Feeling cold or shivering is another possible side effect, often accompanied by a fever.
- Fever:A low-grade fever is common, typically resolving within 1-2 days.
- Nausea:Feeling nauseous or vomiting is less common, but may occur within the first 24-48 hours after vaccination.
Mechanisms Behind Vaccine-Related Side Effects
Vaccine-related side effects are generally a sign that the immune system is working as intended. When a vaccine is administered, it introduces a weakened or inactive form of the virus, or just a piece of the virus, to the body.
This triggers the immune system to produce antibodies that can fight off the real virus if encountered in the future. The side effects experienced after vaccination are often due to the body’s immune response to the vaccine. For example, pain and swelling at the injection site are caused by the body’s inflammatory response to the vaccine.
Fatigue, headache, and muscle aches may be due to the body’s production of cytokines, which are proteins that help regulate the immune response.
Serious Adverse Events
While serious adverse events are rare, they can occur. These are severe reactions that require medical attention and are not simply mild side effects.
- Anaphylaxis:This is a severe allergic reaction that can be life-threatening. It is characterized by symptoms such as difficulty breathing, hives, swelling of the face, lips, or tongue, and a rapid heartbeat.
- Myocarditis and Pericarditis:These are inflammatory conditions of the heart muscle and the lining around the heart, respectively. They have been reported in some individuals, particularly young males, after receiving mRNA vaccines.
- Thrombocytopenia with Thrombosis Syndrome (TTS):This rare but serious condition is characterized by blood clots and low platelet counts. It has been associated with the Johnson & Johnson vaccine.
Vaccine Hesitancy and Misinformation
The widespread adoption of COVID-19 vaccines has been crucial in mitigating the pandemic’s impact. However, vaccine hesitancy, fueled by misinformation and distrust, has posed significant challenges to public health efforts. Understanding the factors contributing to vaccine hesitancy is essential for developing effective strategies to address it.
Factors Contributing to Vaccine Hesitancy
Several factors contribute to vaccine hesitancy, including:
- Misinformation and distrust:The spread of misinformation about vaccines on social media and other platforms has fueled distrust and skepticism. Conspiracy theories, unfounded claims about vaccine side effects, and exaggerated risks have contributed to a climate of fear and uncertainty.
- Lack of access and affordability:Barriers to accessing vaccines, such as limited availability, cost, and transportation challenges, can prevent individuals from getting vaccinated.
- Cultural and religious beliefs:Some cultural and religious beliefs may conflict with vaccination, leading to refusal or reluctance.
- Historical mistrust of healthcare systems:Historical experiences of medical mistreatment or exploitation can lead to distrust in healthcare systems and a reluctance to participate in vaccination programs.
- Lack of trust in authorities:Distrust in government agencies, public health officials, and the pharmaceutical industry can contribute to vaccine hesitancy.
Common Misconceptions and Myths
Misconceptions and myths about COVID-19 vaccines are widespread and often rooted in a lack of understanding of scientific evidence. Some common misconceptions include:
- Vaccines cause autism:This myth, debunked by numerous scientific studies, originated from a fraudulent study published in a medical journal in 1998. The study was retracted, and the author lost his medical license.
- Vaccines contain microchips or tracking devices:This conspiracy theory lacks any scientific basis and is often spread through social media.
- Vaccines are unsafe and cause serious side effects:While vaccines can have side effects, these are typically mild and temporary. The benefits of vaccination far outweigh the risks.
- Natural immunity is better than vaccine-induced immunity:While natural infection can provide some immunity, it can also lead to severe illness, hospitalization, and even death. Vaccines offer a safer and more effective way to develop immunity.
- Vaccines are not effective:Clinical trials and real-world data have consistently shown that COVID-19 vaccines are highly effective in preventing severe illness, hospitalization, and death.
The Role of Public Health Communication
Effective public health communication is crucial for addressing vaccine hesitancy and promoting accurate information. This involves:
- Providing clear and concise information:Public health campaigns should provide accurate, evidence-based information about vaccines in a way that is easily understood by the general public.
- Addressing concerns and misconceptions:Public health officials should proactively address common misconceptions and myths about vaccines, providing evidence-based counterarguments.
- Building trust:Establishing trust with the public is essential. This involves transparency, accountability, and engaging with communities to understand their concerns.
- Utilizing diverse communication channels:Public health campaigns should utilize a variety of communication channels, including social media, traditional media, community outreach programs, and trusted community leaders.
- Promoting community engagement:Engaging communities in discussions about vaccination can help build trust and address concerns.
Future Directions in Vaccine Development
The remarkable success of COVID-19 vaccines has propelled the field of vaccine development into a new era of innovation. The development of novel vaccine technologies, particularly mRNA vaccines, has opened up exciting possibilities for addressing future pandemics and tackling a broader range of diseases.
Emerging Vaccine Technologies
The development of mRNA vaccines has been a significant breakthrough in vaccine technology. This technology utilizes messenger RNA (mRNA) to instruct cells to produce specific proteins that trigger an immune response. mRNA vaccines have several advantages over traditional vaccines, including:* Rapid development:mRNA vaccines can be developed and manufactured much faster than traditional vaccines, as they do not require the cultivation of viruses or bacteria.
Versatility
mRNA vaccines can be easily adapted to target different pathogens, making them highly adaptable for emerging infectious diseases.
Improved safety
mRNA vaccines do not contain live viruses or bacteria, reducing the risk of infection or adverse reactions.Beyond mRNA vaccines, other promising vaccine technologies are emerging, including:* Viral vector vaccines:These vaccines use harmless viruses to deliver genetic material that encodes for the target antigen.
Protein subunit vaccines
These vaccines use purified proteins from the target pathogen to stimulate an immune response.
Nanoparticle vaccines
These vaccines utilize nanoparticles to deliver antigens and adjuvants to enhance immune responses.
Next-Generation mRNA Vaccines
Ongoing research is focusing on developing next-generation mRNA vaccines with enhanced features, such as:* Improved stability:Researchers are working on developing mRNA vaccines that are more stable at room temperature, making them easier to transport and store.
Targeted delivery
New approaches are being explored to deliver mRNA vaccines specifically to target cells, potentially enhancing efficacy and reducing side effects.
Combination vaccines
There is interest in developing mRNA vaccines that can protect against multiple pathogens, providing broader immunity.
Areas of Ongoing Research and Innovation
Several areas of ongoing research and innovation are shaping the future of vaccine development:* Personalized vaccines:Scientists are exploring the development of personalized vaccines tailored to an individual’s genetic makeup and immune response.
Universal flu vaccines
Researchers are working on developing a universal flu vaccine that would provide protection against a broad range of influenza strains.
Vaccines for cancer and other diseases
mRNA vaccines are being investigated for their potential to treat cancer and other chronic diseases.
Vaccine delivery systems
New delivery systems, such as micro-needles and nasal sprays, are being developed to make vaccines more accessible and convenient.
The future of vaccine development is bright, with the potential to transform global health and disease prevention.
Last Word
The journey to understand COVID-19 vaccines has been a fascinating one, full of scientific breakthroughs and ongoing research. While mRNA vaccines have captured the spotlight, it’s important to remember that a diverse range of technologies contribute to our arsenal against this virus.
By understanding the different types of vaccines and their mechanisms, we can make informed decisions about our health and contribute to a more informed public discourse about these crucial medical interventions. As we move forward, continued research and innovation will undoubtedly lead to even more effective and accessible vaccines for future pandemics.