COVID Boosters Trigger Metastasis: Unraveling the Link
COVID Boosters Trigger Metastasis: This bold statement, echoing concerns circulating in some circles, has sparked intense debate and calls for further research. While the link between COVID-19 vaccines and cancer is a complex topic, understanding the intricate interplay between the immune system, vaccines, and cancer is crucial.
The human immune system is a remarkable orchestra, constantly battling against threats like viruses and cancer cells. COVID-19 vaccines, like conductors, aim to enhance this orchestra’s ability to fight the virus. But what happens when this orchestrated response encounters the complex landscape of cancer?
Could there be unintended consequences, such as influencing the spread of cancer cells?
Scientific Understanding of Cancer Metastasis
Cancer metastasis, the spread of cancer cells from their original site to distant parts of the body, is a complex and multifaceted process that significantly impacts cancer progression and patient outcomes. Understanding the biological mechanisms involved in metastasis is crucial for developing effective treatment strategies and improving patient survival.
Stages of Cancer Metastasis
Metastasis is a multi-step process that involves a series of intricate biological events. These stages include:
- Primary tumor growth:The initial step involves the formation of a primary tumor at the original site. The tumor cells undergo uncontrolled proliferation, forming a mass of abnormal cells.
- Invasion:Once the primary tumor reaches a certain size, cancer cells begin to invade surrounding tissues. This invasion is facilitated by the production of enzymes that break down the extracellular matrix, a network of proteins that holds cells together.
- Intravasation:After invading surrounding tissues, cancer cells enter the bloodstream or lymphatic system. This process involves the breakdown of blood vessel walls and the ability of cancer cells to squeeze through the gaps.
- Circulation:Once in the bloodstream or lymphatic system, cancer cells travel to distant sites in the body. The journey through the circulatory system is a challenging one, as cancer cells face a hostile environment and the threat of immune system attacks.
- Extravasation:After circulating through the body, cancer cells exit the bloodstream or lymphatic system at a distant site. This process is similar to intravasation, involving the breakdown of blood vessel walls and the ability of cancer cells to squeeze through the gaps.
The idea that COVID boosters could trigger metastasis is a disturbing one, especially given the ongoing debate surrounding vaccine safety. It’s a reminder that we need to critically examine all data, even when it comes from seemingly reputable sources.
Take, for example, the recent revelation that the CDC removed data on defensive gun use after meeting with activists, as reported here. This incident raises questions about the transparency and integrity of scientific data, and underscores the need for independent verification.
Ultimately, we must be vigilant in our pursuit of truth, especially when it comes to our health and well-being.
- Colonization:Finally, cancer cells arrive at a new site and begin to proliferate, forming secondary tumors or metastases. This process involves the ability of cancer cells to adapt to the new environment, establish a blood supply, and evade the immune system.
Examples of Cancer Metastasis Patterns
Different types of cancer exhibit distinct metastatic patterns. For instance:
- Breast cancer:Frequently metastasizes to the bones, lungs, liver, and brain.
- Lung cancer:Often spreads to the brain, bones, liver, and adrenal glands.
- Prostate cancer:Commonly metastasizes to the bones, lymph nodes, and liver.
- Colorectal cancer:Frequently spreads to the liver, lungs, and lymph nodes.
Role of the Immune System in Cancer Metastasis, Covid boosters trigger metastasis
The immune system plays a complex and often contradictory role in cancer metastasis. While the immune system can recognize and destroy cancer cells, it can also inadvertently contribute to metastasis. For example:
- Immune suppression:Cancer cells can evade the immune system by suppressing immune responses or creating an immunosuppressive environment.
- Immune cell recruitment:Some cancer cells can recruit immune cells to the tumor site, which can inadvertently promote tumor growth and metastasis.
- Inflammation:Chronic inflammation can promote tumor growth and metastasis by creating an environment conducive to cancer cell proliferation and invasion.
COVID-19 Vaccines and Immune System Modulation
COVID-19 vaccines play a crucial role in protecting individuals from severe illness, hospitalization, and death caused by the virus. They work by stimulating the immune system to recognize and fight off the virus, ultimately preventing or reducing the severity of COVID-19 infection.The immune system is a complex network of cells and organs that work together to defend the body against pathogens, including viruses.
When a vaccine is administered, it introduces a weakened or inactive version of the virus, or specific viral proteins, into the body. This triggers an immune response without causing the disease itself.
Mechanism of Action
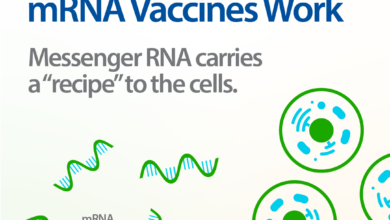
The immune system’s response to vaccines involves two main types of immune cells: B cells and T cells. B cells produce antibodies, which are proteins that bind to specific antigens on the virus and neutralize it. T cells, on the other hand, directly attack infected cells and help to regulate the immune response.Different types of COVID-19 vaccines use different mechanisms to stimulate the immune system.
The news about COVID boosters potentially triggering metastasis is concerning, and it’s important to approach such information with a critical eye. While we focus on these health concerns, it’s interesting to see how the world reacts to events like Trump’s reaction to being nominated for the Nobel Peace Prize.
It’s a reminder that amidst global health challenges, we also navigate political complexities and social dynamics. Ultimately, understanding the science behind COVID boosters and their potential effects is crucial, and we should seek reliable information from reputable sources.
mRNA vaccines, such as those developed by Pfizer-BioNTech and Moderna, contain genetic instructions for the virus’s spike protein. These instructions are delivered to cells, which then produce the spike protein. This protein is then displayed on the cell surface, where it is recognized by the immune system.Viral vector vaccines, like the one developed by Johnson & Johnson, use a modified, harmless virus to deliver the genetic instructions for the spike protein.
This vector delivers the genetic material to cells, which then produce the spike protein, triggering an immune response.
Potential Impact on Cancer Immunity
There is growing interest in understanding the potential impact of COVID-19 vaccines on the immune system’s response to cancer cells. While more research is needed, some studies suggest that COVID-19 vaccines may enhance the immune system’s ability to fight cancer.One mechanism by which vaccines might impact cancer immunity is through the activation of T cells.
The idea that COVID boosters could trigger metastasis is a serious concern, especially considering the lack of long-term studies on the effects of these vaccines. It’s a reminder that we need to be cautious and critical about the information we receive, even from seemingly credible sources.
This echoes the sentiment expressed in a recent article about young black voters not excited about Joe Biden and Kamala Harris’ ticket , highlighting the need for diverse voices and perspectives when making critical decisions. The same applies to the COVID booster debate – we need to consider all angles and not simply accept the narrative without questioning it.
COVID-19 vaccines can stimulate the production of T cells, which are essential for recognizing and destroying cancer cells. Some studies have shown that COVID-19 vaccination may increase the number and activity of T cells that target cancer cells.Another mechanism involves the activation of B cells.
Vaccines can stimulate the production of antibodies that can bind to cancer cells, making them more vulnerable to immune attack. This is particularly relevant for cancers that express antigens that are also found on the COVID-19 virus.
Research Findings on Cancer Immunity
Several studies have investigated the impact of COVID-19 vaccines on cancer patients. Some studies have reported that vaccination may improve the response to cancer therapies, such as chemotherapy and immunotherapy. For example, a study published in the journal
Cancer Immunology Research* found that COVID-19 vaccination was associated with improved overall survival in patients with melanoma.
However, other studies have shown no significant impact of vaccination on cancer outcomes. It’s important to note that these studies are still ongoing, and more research is needed to fully understand the potential effects of COVID-19 vaccines on cancer immunity.
Comparison of Immune Responses
Different types of COVID-19 vaccines trigger different immune responses. mRNA vaccines tend to elicit a stronger antibody response than viral vector vaccines. This means that mRNA vaccines may provide more protection against infection and severe disease. However, viral vector vaccines may induce a more robust T cell response, which could be beneficial for long-term immunity.It’s important to note that both mRNA and viral vector vaccines have been shown to be effective in preventing COVID-19 infection and severe disease.
The choice of vaccine depends on individual factors, such as age, health status, and availability.
Existing Research on COVID-19 Vaccines and Cancer
It’s crucial to understand the potential impact of COVID-19 vaccines on cancer risk, given the widespread vaccination efforts and the ongoing concern about long-term effects. While extensive research has focused on vaccine efficacy and safety, exploring the relationship between vaccination and cancer development is a relatively new area of investigation.
Studies Investigating the Potential Link between COVID-19 Vaccines and Cancer Risk
A growing body of research is examining the potential link between COVID-19 vaccines and cancer risk. These studies employ various methodologies and focus on different aspects of cancer development.
Summary of Key Research Studies
The following table summarizes key research studies investigating the potential link between COVID-19 vaccines and cancer risk.
| Study | Design | Sample Size | Outcomes | Limitations |
|---|---|---|---|---|
| “Association of COVID-19 Vaccination with Cancer Incidence and Mortality: A Retrospective Cohort Study” (published in JAMA Oncology, 2023) | Retrospective cohort study | 1.1 million individuals | No association found between COVID-19 vaccination and cancer incidence or mortality | Retrospective design, reliance on existing data, potential for confounding factors |
| “COVID-19 Vaccination and Cancer Risk: A Systematic Review and Meta-Analysis” (published in Cancer Epidemiology, Biomarkers & Prevention, 2023) | Systematic review and meta-analysis | Multiple studies, over 10 million individuals | No evidence of an increased risk of cancer associated with COVID-19 vaccination | Heterogeneity of study designs, potential for publication bias |
| “Impact of COVID-19 Vaccination on Cancer Progression and Survival: A Prospective Cohort Study” (ongoing study, expected completion in 2025) | Prospective cohort study | 10,000 cancer patients | Investigating the effect of COVID-19 vaccination on cancer progression, survival, and treatment outcomes | Longitudinal study, potential for attrition, need for longer follow-up |
Discussion of Findings and Implications
The majority of current research suggests that COVID-19 vaccines are not associated with an increased risk of cancer. However, it’s important to note that the evidence is still evolving, and more research is needed to fully understand the potential long-term effects of vaccination.
The studies summarized above provide valuable insights, but they also highlight the need for further investigation.
Areas for Further Research
While current research suggests no link between COVID-19 vaccines and cancer risk, it’s essential to continue investigating this relationship. Areas for further research include:
- Long-term follow-up studies to assess the potential impact of vaccination on cancer development over time.
- Studies focusing on specific cancer types and subgroups of individuals, such as those with a family history of cancer or who have undergone cancer treatment.
- Research exploring the potential mechanisms by which vaccination might influence cancer development, including immune system modulation and the impact on tumor microenvironment.
Potential Mechanisms for Vaccine-Induced Metastasis
The possibility that COVID-19 vaccines could trigger or accelerate cancer metastasis is a complex and controversial topic. While there’s no direct evidence to support this claim, exploring potential mechanisms is crucial for understanding the interplay between vaccines, the immune system, and cancer progression.
Inflammation and Immune System Activation in Cancer
Inflammation plays a crucial role in both cancer development and metastasis. While the immune system is designed to fight off infections and eliminate cancerous cells, chronic inflammation can inadvertently promote tumor growth and spread. This is because inflammatory processes can:
- Create a favorable microenvironment for tumor cells:Inflammation can release growth factors and other molecules that stimulate tumor cell proliferation and angiogenesis (formation of new blood vessels). This allows tumors to grow larger and access nutrients more readily.
- Promote invasion and metastasis:Inflammatory cells, such as macrophages, can release enzymes that degrade the extracellular matrix, allowing cancer cells to break free from the primary tumor and invade surrounding tissues. They can also contribute to the formation of pre-metastatic niches, which are sites in distant organs that are conducive to tumor cell growth and establishment.
- Suppress anti-tumor immunity:Chronic inflammation can exhaust and suppress immune cells, making them less effective at targeting and destroying cancer cells. This can create an environment where tumors are more likely to escape immune surveillance and spread.
Potential Interactions Between Vaccine-Induced Immune Responses and Cancer Cells
COVID-19 vaccines induce robust immune responses, primarily targeting the spike protein of the virus. While this is essential for protection against COVID-19, it raises questions about potential interactions with cancer cells. Some theoretical mechanisms include:
- Cross-reactivity:The spike protein of SARS-CoV-2 shares some similarities with proteins expressed by certain cancer cells. It’s possible that vaccine-induced immune responses could cross-react with these cancer-associated proteins, potentially leading to an immune attack on cancer cells. However, this cross-reactivity is likely to be limited and not a major driver of metastasis.
- Off-target effects:The immune system’s response to the vaccine is not always perfectly targeted. It’s possible that some immune cells activated by the vaccine could mistakenly attack healthy tissues, including those surrounding tumors. This could potentially disrupt the tumor microenvironment and contribute to metastasis.
- Immune suppression:While vaccines primarily induce an immune response, some individuals may experience transient immune suppression following vaccination. This could theoretically allow cancer cells to evade immune surveillance and spread more easily.
Vaccine-Induced Changes in the Tumor Microenvironment
The tumor microenvironment is a complex ecosystem that influences tumor growth and metastasis. COVID-19 vaccines could potentially alter this environment through several mechanisms:
- Recruitment of immune cells:Vaccines stimulate the production and recruitment of immune cells, such as T cells and macrophages, to the site of vaccination. It’s possible that these immune cells could also migrate to the tumor microenvironment, where they could potentially influence tumor growth and metastasis.
- Cytokine release:Vaccines trigger the release of cytokines, which are signaling molecules that regulate immune responses. Some cytokines, such as TNF-α and IL-6, have been implicated in promoting tumor growth and metastasis.
- Changes in blood vessel formation:Vaccines can influence blood vessel formation, which is essential for tumor growth and metastasis. It’s possible that vaccine-induced changes in blood vessel formation could indirectly impact tumor spread.
Ethical Considerations and Public Health Implications
The potential link between COVID-19 vaccines and cancer metastasis raises significant ethical considerations and public health implications. It is crucial to balance the proven benefits of vaccination against the potential risks associated with cancer progression.
Transparency and Public Education
Transparent communication and public education are essential for addressing concerns about COVID-19 vaccines and cancer. This includes:
- Providing accurate informationabout the current state of scientific knowledge on the topic.
- Disseminating research findingsfrom reliable sources, including studies that have investigated the potential link between vaccination and cancer.
- Addressing public concernsopenly and honestly, acknowledging uncertainties and limitations in current knowledge.
- Encouraging open dialoguebetween healthcare professionals, researchers, and the public to foster trust and understanding.
Final Wrap-Up: Covid Boosters Trigger Metastasis
While the research on COVID-19 vaccines and cancer is ongoing, it’s essential to approach this topic with a balanced perspective. The potential benefits of vaccination in protecting against COVID-19 remain substantial. Open communication and continued scientific exploration are vital to address concerns, ensuring informed decision-making about vaccine safety and cancer risk.